Fever Of Unknown Origin – FUO
It’s called FUO or “Fever of Unknown Origin” and its definition is about as big a mystery as its name. Back during my medical school days FUO meant something different to the neonatologists in the newborn unit than it did to the pediatricians out on the hospital ward.
FUO, Fever of Undetermined Origin
Then, when you added all the private “attendings” who admitted patients and the definitions they used, we residents had a hard time keeping up. One of the nurses even posted a list of what definitions each doctor in the community seemed to use—and some of them even had ranges for temperature and duration (meaning he had no solid definition.)
Some kids we saw were really sick, others less so; but, they were all a diagnostic dilemma—that’s what they all seemed to have in common. Everyone knew they were “sick” because they had a fever; but, the: “with what” was the mystery—FUO!
Even the kids who didn’t appear to be sick had parents who feared they were; because, kids aren’t supposed to have fevers unless they are sick!
A Child With Fever of Undetermined Origin
Where diagnostic skills meet the road
For a pediatric resident trying to learn the skill of recognizing illnesses it’s nothing to joke about. Which is why we tended to cringe a bit when an attending would answer one of our incessant and difficult questions with: “Well, they just look sick!”
That’s about as helpful as the dip-stick coach who tells his player: “if you’re not bleeding it’s not that bad so quit whining.”
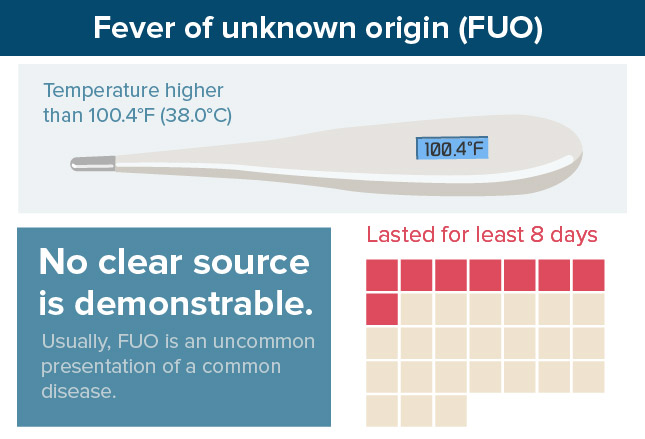
But what does “sick” look like to you? For that matter, what do you consider an actual fever: 100.4°F (38.0°C)? 101°F (38.3°C)? And how long is too long? Five days? Twenty-one days?
FIRST the Definitions
There is no place on earth where the words “there are exceptions to every rule” applies more than in medicine.
That’s why we’ve had such a hard time fixing on a definition for FUO; but time, experience and sheer necessity seems, in pediatrics at least, to have us focused on: “a fever at least between 100.4-101°F which has lasted for at least 8 days and for which no clear source.”
Age Matters
I said neonatologists see the world differently than the rest of us. That’s because A N Y fever in an infant under 3 or 4 months IS SEEN AS A CRISIS which can’t wait around for some rash to develop and must be diagnosed quickly.
Treatment can’t wait and, in that age range, is often begun even before the diagnosis is evident. That’s because neonates haven’t yet developed their immune system so can’t fight off infections on their own.
The mantra in the Newborn ICU is: “It’s Sepsis until proven otherwise.” Sepsis meaning that bacteria has already invaded the blood stream. If the newborn, even in the slightest, doesn’t act “normal” for the situation they have cultures taken of everything and antibiotics started as soon as an IV line can be established.
Yes, we know that a lot of the time that is a bit of an over-reaction; but, it isn’t really. Perhaps it is the single greatest contributor to the low infant mortality in developed countries and the greatest reason most women who are able, choose not to deliver at home.
So, age does matter and the rest of this discussion is ONLY about older children, not neonates. The term “FUO” which we are discussing now, really just doesn’t apply to newborns.
Uncommon Things Happen Uncommonly
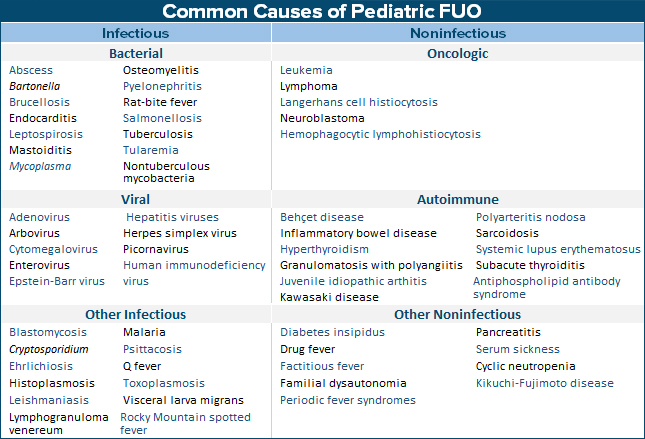
You may have to click on the image to expand and be able to read it; but, the list of “common causes of Pediatric FUO” contains a lot of names that are hard to pronounce and other oddities.
Lucky for us the reason most of you haven’t heard of most of them is because: “common things happen commonly,” and these are not in that group. And just as lucky that: usually an FUO turns out to be “an uncommon presentation of a common disease” which is just taking its own sweet time doing what it does.
I can tell you from first-hand experience that by the seventh day, when a six-year-old has a fever of 104° without showing any other symptoms, it’s not ONLY his parents who are fit-to-be-tied, his grey-haired doctor isn’t sleeping too well either!
Six times now for me, exactly like that, we were all sweating bullets; when, on the eighth day, blisters erupted in the child’s mouth and we knew it was “primary herpes stomatitis.”
Until then, we had been gradually ratcheting up the worry, admission to the hospital, laboratory studies and safely trying to “cover all bases.”
You see, that’s the way the Herpes Simplex virus works. The first attack is a full-blown knock out and after that you just get a “cold sore” when you get run down or stressed.
Let me give you a couple more examples showing the range of issues we’re dealing with in an FUO:
Four-year-old, 7 day fever

A previously completely healthy 4-year-old- girl emigrated from India with her parents 12 days ago and she’s already been to EDs and Urgent Care FOUR times in the past 7 days with fever and abdominal pain. All vaccinations are current for India including hepatitis A and B plus Typhoid. She is due for a typhoid booster soon.
Today, your office staff is able to “work her in” because of blood in her stool for two days and she, finally, gets a good (i.e. complete) exam which found that she has a slightly enlarged liver and mild abdominal tenderness—but her lab work is “sicker” than she appears.
The thing is, if they had gone to almost any “doctor” in India she would have been diagnosed and treated on the first visit! As it was, four different U.S. “practitioners” failed to even think of a disease which causes 33 MILLION cases and half a MILLION deaths in the world every year! The US has about 300 reported cases each year.
The simple stool culture that you took (shown) eventually grew out: Salmonella Thyphi—Typhoid Fever or Enteric Fever.
In this case the infection had spread from the intestinal tract into the blood stream causing the fever, pain and eventually diarrhea. Luckily, she hadn’t progressed to perforation or neurologic abnormalities and didn’t develop the rash—perhaps due to the partial immunity from her shots.
An FUO demands a more than an “automated” (and largely ignored) complete Review Of Systems and History Of Present Illness.
Six year old, 9 day fever
This reported case, unfortunately, doesn’t represent physicians at their finest hour. A 6-year-old boy developed a fever without other symptoms and was seen by his practitioner where an “ear infection” was diagnosed (even though an earache was not a complaint)—and even worse, antibiotics were begun.
Nine days into the illness, still with fever, he was seen again having developed lateral thigh pain that morning. It wasn’t stated what happened at that visit, only that the next day (10th fever day) he developed knee pain and his doctors office told them to go to the emergency room to be seen.
It was claimed that his exam was “normal” but extensive laboratory tests showed basically that “his body was fighting off an infection somewhere” even though x-rays of pelvis, femur, knee and tib/fib were normal. They also chose to do an MRI of the knee which was normal.
We were told that still “a few days later” (one would surmise three or more) although “examination findings” remain normal, the patient continued to have a fever, and his blood work still showed an infection.
Blood cultures had not grown any organisms—which they usually don’t once ANY kind of antibiotics have been started. A huge reason NOT to be so cavalier with antibiotics.
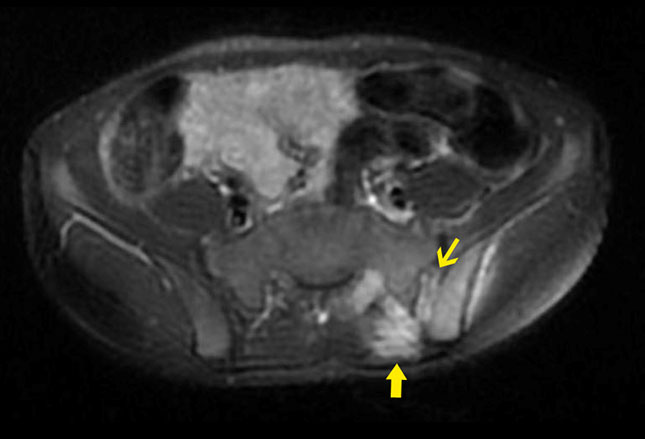
Finally, an MRI of the pelvis and the entire left lower extremity was ordered and someone took a history about pets which was positive for cats (multiple).

The MRI showed a big problem with infection in his hip; which, the report stated, prompted the doctors to go back and do a complete physical exam which actually revealed that he did have pain in his hip. AND, several cat scratches!
Several “spots” of bone infection of the hip joint with a large abscess was revealed on the MRI which was then drained. Eventually blood work did show the infection was due to “cat scratch disease” and the boy was treated. The third most common infectious cause of FUO in children.
An FUO demands a good physical exam, the kind they taught you to do in medical school!
14 year-old, 8 days fever with knee pain
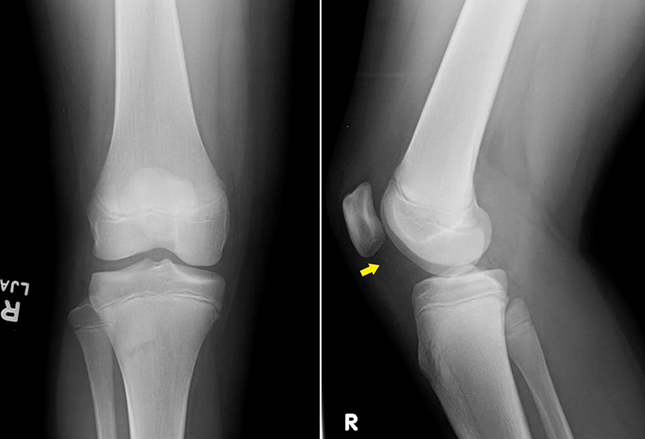
In another reported case, a 14-year-old boy was seen by his “primary care physician” with 8 days of fever and right knee pain without any antecedent injury or plausible explanation (that sort of makes this a suspicious case.)
A good physical revealed warmth and tenderness in his femur with limitation of motion due to pain. X-rays did show fluid in the joint (arrow) and soft tissue swelling which could be an infection; but, the blood work showed something else.
There were lots of white blood cells in his blood work with immature forms and evidence of increased cell destruction but not a significant inflammatory process.
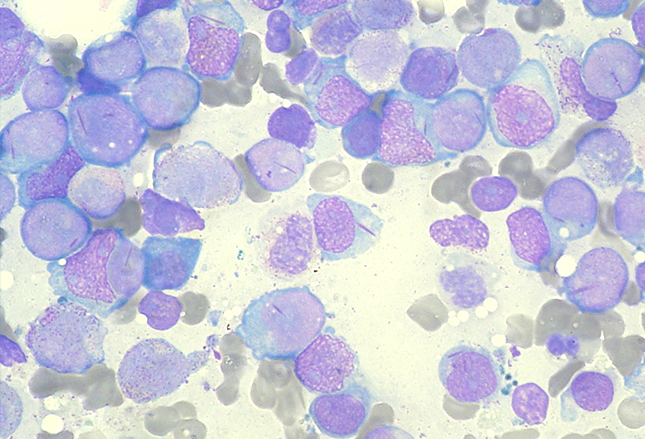
The next step was to do a bone marrow biopsy (shown) which showed a leukemic infiltrate consistent with acute myeloid leukemia.
Acute leukemia is the most common cancer in children. Initial presenting symptoms may be nonspecific and may include fever, malaise, musculoskeletal pains, lymphadenopathy, hepatosplenomegaly, and bleeding. The high index of suspicion this doctor had led to a rapid diagnosis and proper treatment.
An FUO demands that a physician not get “locked in” to an “easy” diagnosis and follow any unusual leads.
15 month old, 8 day fever
Babies, especially those with older siblings often get fevers with illnesses; however, even in those instances, 2-4 days is the norm.
This 15 month old has had a fever for 8 days and already has had a chest x-ray, blood work and urine testing without finding a source for her fever. Four days previous a lump developed on her neck, two days previous she developed red eyes, lips, tongue, hands and feet and had a rash on her abdomen.
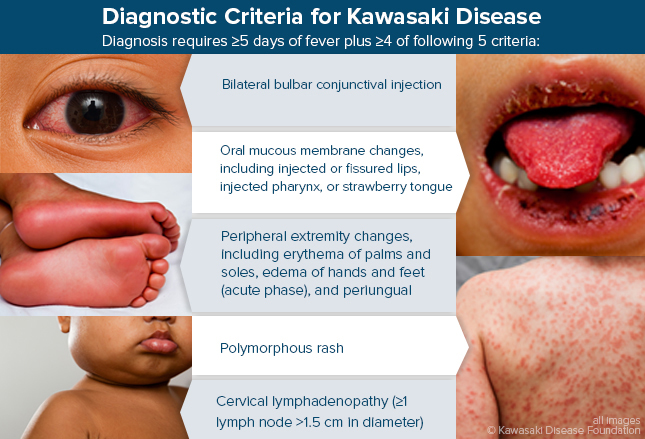
Laboratory testing today shows general evidence of bodily inflammation, a slightly low white count and slightly elevated platelet count—the (fairly) classic presentation of Kawasaki’s Disease, an inflammation of the medium-sized muscular arteries.
It predominantly attacks children and can lead to serious heart issues if not treated promptly. In fact, it’s the leading cause of acquired heart disease in U.S. children—and is still without a known cause.
Truly, the disease is a bit difficult to diagnose because so many other common problems have similar findings; but, a fever lasting more than 5 days with a “rash” on the hands and palms should have caused her doctors to at least consider it several days earlier if they had seen her and examined her fully. (See chart)
Treatment is a bit difficult and careful followup for heart disease is critical watching for coronary aneurysms.
An FUO demands that a patient be given a “streamlined” access to speak directly with the physician without “triage” by appointment-making office personnel; and, that parents and care-givers be persistent in being seen—daily, if necessary, until a diagnosis is known. Especially after 5 days.
5 year old, 2 month fever
A report states that this 5-year-old girl, residing in Mexico, has had a daily fever for at least 2 months. This was on top of left knee pain for a year for which she was diagnosed as “juvenile idiopathic arthritis.”
Despite being treated with both methotrexate and prednisolone (powerful meds with side-effects) she hasn’t been able to walk for the past 6 months and has lost 17 kilograms (37 pounds) over the last month!
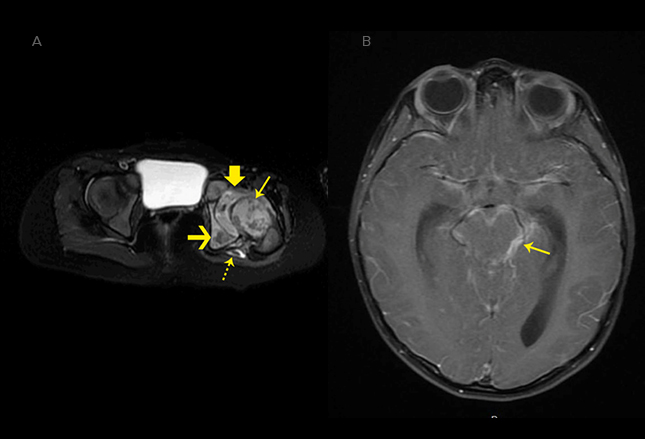
She’s now had a daily right-side headache for 5 days and begun vomiting with fatigue and confusion. Physical exam showed an emaciated child at the 1st percentile for weight and 4th percentile for height. She holds her right hip and knee at full flexion and refuses any attempt at motion.
An MRI (left leg and brain) was obtained which showed osteomyelitis of nearly all the bones in the left hip and an abscess consistent with tuberculosis which, unfortunately, has now also spread to cause meningitis of the brain.
The diagnosis was confirmed by a spinal tap and biopsy of tissues in the hip where “acid-fast” bacilli (the Mycobacteria tuberculosis organisms) were found. Just as unfortunately, the report doesn’t say whether the simple Tb Tine scratch or intradermal PPD test was ever done back when her fever began or their results.
These should have been done before the diagnosis of arthritis was made, especially prior to initiating chronic medications in a child; and, unless contraindicated, re-done at any or several times when it was clear the heavy medications weren’t working.
Children are especially prone to the spreading of Tuberculosis organisms throughout the body; and, the medications that were given make the body less able to fight off infections.
An FUO demands that not only unusual causes be considered but that physicians take charge of reviewing all laboratory results to make sure they have been done accurately and even repeated if necessary as the fever continues.
☤
Fortunately, FUOs aren’t commonly seen. Fortunately, when they are they are most often “uncommon presentations of common illnesses.” Unfortunately, even though rare, they can be a harbinger of something very serious. And they nearly always make highly visible even the smallest deficiency or complacency in a physician’s procedures or practices.

