10 Scary Issues About Concussions
I saw a 5-year-old purple-faced dragon at Sam’s Club trying to go ingognito. She was wearing the lace-up pink boots that everyone knows is what frogs wear when they want to go out on the town. She couldn’t fool me!
Concussion: not an easy fix
Then it dawned on me that Halloween (in the states) was upon us again – football season (American) winding down, basketball starting, turkeys getting nervous and a whole new set of injuries starting to fill the ER guerneys – including concussions and other head injuries.
This is one area where what we thought we knew was only a mere thimble-full compared to what we are beginning to realize – and to what we are afraid me might learn.
Perusing a recent Morbidity and Mortality Weekly Report (MMWR) [2014;63:352-355, 362-363] got me to thinking that much of what we see as doctors is needlessly inflicted on children, merely through inadequate information. OK, there are some yahoo’s whose tunnel-visioned motivations clearly only involve trophies at the expense of a child; but, fortunately they are still in the minority.
All the media attention about the high-profiled, brain-injured professionals has made parents worried – and rightly so; but, in some ways not worried enough.
Let me list ten scary issues about children’s concussions. At least they worry me and I’m hoping my worries rub off on you.
The Ten Issues About Concussion To Be Afraid Of
The American College of Sports Medicine (ACSM) is the bunch of medical specialists board certified in Sports Medicine who track amounts and causes of injuries related to all sports in all ages.
They tally 300,000 sports and recreation-related concussions in the U.S. every year; BUT, they also estimate that the REAL number is seven times more than that! That would be 2.1 MILLION concussions every year! That is because their specific data from schools and leagues prove that only one in seven concussions are actually reported or seen by physicians.
So, here are our worries:
Returning to play too soon
Getting a concussion is a tiny bit like playing black-jack BUT really not! Normally you draw from a deck where every draw has an equal chance of occurring so you can quit while you are ahead.
Concussions are a completely different story however. Once you get one it’s like then taking everything except face cards out of the deck – taking even one more card almost always means you bust! Like playing Russian Roulette with only one chamber empty!
Having your “bell rung,” “seeing the shineys” or “taking a ‘rest’ on the field” (getting a concussion) opens a “window of vulnerability” of the brain in which the next “bump,” no matter how otherwise tiny and insignificant, can have literally a life-devastating effect. That’s what you’re hearing more and more about it in the press.
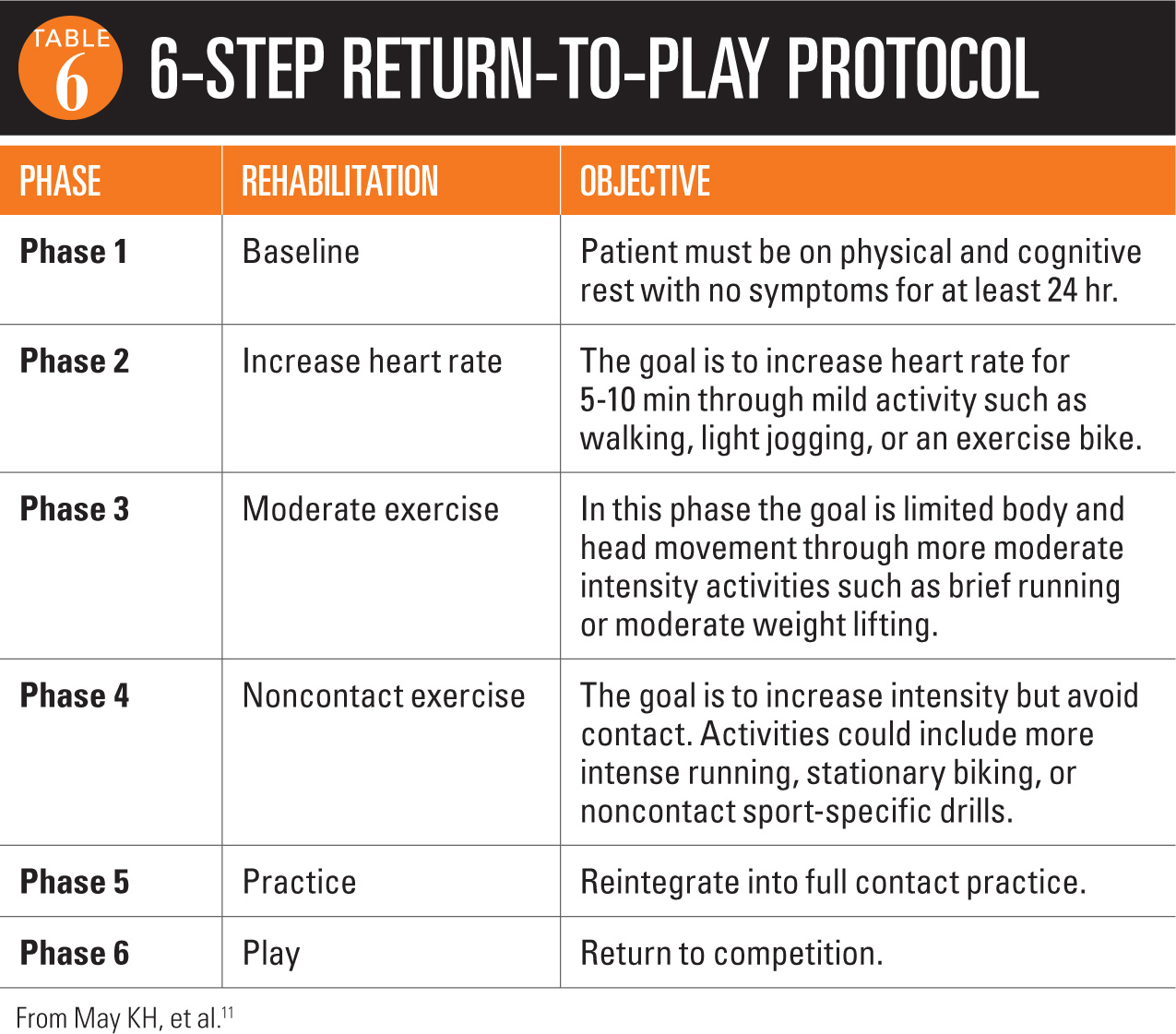
The issue is that we all know the window’s open after a concussion but there is no test to tell when it closes and you are “safe” again! The new Neuro-cognitive testing techniques MAY give hints about when a concussion has occurred but cannot reveal anything about return to play (RTP).
Each concussion is different just as each brain is different so the only logical approach is to use guidelines designed to keep children as safe as possible – it is only a game after all.
Every bit of the new information we are learning reveals that we’ve been terribly cavalier with the well being of our children, that we’ve been terribly inadequate in both diagnosing and treating concussions and that the consequences are consistently more significant and severe than we’ve ever realized.
Improper technique
The techniques we’re talking about involve… heads. Incredibly, now that we think about it, coaches have taught children to use their heads as a weapon. “Stick him,” “helmet him in the numbers” and “go root-hog him (dive at an opponent’s feet)” are all now instructions that coaches deny ever issuing and are fodder for lawsuits if they ever do.
An analysis of the location of players’ heads during the game may bring caring parents to their feet in most plays and certainly reveals the dangers in football, ice hockey, lacrosse and several other sports. And a more specific explanation is given in a news article from the Dayton News. It’s a bit specific and will make sense to most coaches.
Old habits and methods die extremely hard, especially in sports – both coaching and playing. But, they’ve just got to die. Too much depends on it.
Poor Rules Enforcement by Coaches and Officials
Dangerous use of a player’s head has been against the rules for many years; yet, when was the last time you’ve ever seen officials make that call? They very rarely do.
Unsportsmanlike conduct penalties for illegal hits to the head are now beginning to increase as clear-cut damage to players have led to widely publicized injuries and deaths – and the lawyers have become involved.
It’s more important than ever for parents to attend their children’s games.
Concussion Legislation
For a couple of years now, legislators have been wielding their swords; frankly, sometimes to responsibly service communities and sometimes to merely further their own political career.
Athletic trainers (ATs) and physical therapists (who most often are on the front lines) shouldn’t be frightened of good legislation but often see a loss of their return-to-play (RTP) authority as a threat to their income. They are on the front line and most sports wouldn’t be the same without them; but, they are not in a position or trained to make that medical assessment – we now know it’s too critical.
RTP decisions must be made very conservatively, by qualified (and trained) health care providers who have no financial or untoward “pressures” that might return a player too early. Usually coaches, parents and players themselves provide all the pressure needed to hurry the decision and there must be an “unbiased” party to provide the necessary perspective.
Good legislation shouldn’t exclude youth sports or recreational athletes and it must not be so poorly written that it can’t adapt to new knowledge about concussions and treatments.
Sometime back the Milwaukee Journal Sentinel published a review of pending legislation in Wisconsin which might give you the essence of the issues. They pointed out that athletes younger than 11 years old weren’t covered by the proposed legislation even though children are clearly starting a sports career at age 5 to 7-years-old.
Doctors with out of date concussion knowledge
The more training a health provider has undergone the greater the expectation is that they have up-to-date knowledge and the more credibility their opinions are given. Unfortunately, as in many other things, that is not always the case.
To provide you with another side of the coin felt by some ATs is this article describing a specific instance where an ER physician was NOT the most trained or creditable and gave advice that put the child in jeopardy.
The AT who wrote the article states that “most ATs in the traditional setting, especially in the high school, have been given notes by concussed athletes who were treated by a physician who clearly didn’t know what they were dealing with.”
I can’t attest to his observation but I can tell you that IF the ED physician told the parents that it couldn’t be a concussion if the imaging studies (of any type) were negative he/she was absolutely and totally wrong! “Concussion” is NOT a diagnosis made by imaging and physicians know that.
Parents: Denial
From a physicians standpoint, there is less difference in talking to parents about cancer and concussion than you would think. While sports and cancer are clearly worlds apart in importance, sometimes removing a child from sports participation is met with intense denial and opposition from not only the athlete but his parents (usually dad) as well.
“But it’s only a mild concussion“ is often the rebuttal they use which reveals an unfortunate lack of understanding of the issues. There is NO SUCH THING AS A MILD CONCUSSION any more than a person can be “a little pregnant.” ANY concussion is DAMAGE TO THE BRAIN, even if there is no fracture or observable damage on imaging studies.
The ONLY issue is how much and what type of rest/rehabilitation will minimize the damage already sustained. Denial prevents adequate treatment and places a child’s future in jeopardy. So does overreaction.
Fortunately there seems to be less and less of these types of parents now that public understanding is increasing; but physicians still approach a parent quite gingerly when speaking with them about such injuries.
Coaches: Pressure to win
Most coaches will tell you that their job is two-fold: To teach and to motivate – how to do it and to want to do it. Many also admit that teaching is the easiest and motivating takes the most effort.
Those, of course, are both “methods” and don’t address the “purpose.” If you ask “why are we playing this game?” or “Why are we in this tournament?” only “little league” coaches may be bold enough to claim “to have fun” – especially if there are mothers present. That kind of utterance from a school or professional coach would just sound plane silly.
“To showcase and exercise our skills and abilities to the greatest extent possible” may be the politically correct rhetoric they say to the microphone but what they understand – and perhaps worry about – in their hearts is more on the order of “to see which coach has the best players and who has taught and motivated them the best.”
We can understand the pressures because we face them in our lives too, both internal and external. The only problem is to not admit they are there which prevents implementing procedures and safeguards that prevent inappropriate decisions being made based on the pressures!
When a pivotal player suffers a concussion, the coach could turn that pressure towards the Athletic Trainer – or the AT to the athlete – to get them back on the field.
Players who aren’t honest about their symptoms
As disgusting as it sometimes was, the TV series “House” publicized widely the phrase “patients always lie” and showed us the result by damaging them further and further until the diagnosis was revealed … or the patient died, whichever came first.
The myriad of disagreeable consequences for lying to their doc aren’t usually understood by patients (especially children) so I’m afraid lying is common – or at least hiding, omitting or minimizing the truth.
It would be nice if all coaches and ATs could be counted on at all times to not only have but exercise and teach how to keep their sport and games in perspective compared with a child’s life, health and future; but, it would be unreasonable to expect it will happen 100% – given all the pressures. It is clearly up to parents to teach children decision making and priorities: fun and games vs. body, health and life.
Even with advances in concussion research and such things as neuro-cognitive testing by computer, return to play decisions are still highly dependent on the athlete’s symptoms. The strong desire to be on the field that most athletes have tempts them to deny or minimize symptoms, making concussion diagnosis and proper rehabilitation very difficult for coaches, ATs and parents – and making the role of the unbiased physician more critical.
Multiple Concussions
A concussion, no matter how transient the symptoms, means damage to the neurons of the brain. Recovery may be rapid or slow, easy or difficult, complete or partial; BUT, the one thing we’re learning for certain is: “The next head injury will be a lot easier to occur and more significant.”
The “window of enhanced vulnerability to further injury” and “additive neural damage” are concepts verified by almost all research studies and entirely change the way we should look at “sports.”
Knowing when to quit participating in a sport or to retire from the game is a tough decision. A newspaper in Central Maine, The Sentinal, did a feature story on Travis Lazarczyk who at 24 suffers from post-concussion syndrome following 22 of them. Much of a competitive-athlete’s personal identity is wrapped into their sport which can make the decision to retire from sports a psychologically devastating decision.
Public Ignorance
Despite more research on the subject than ever before and the high level of publicity on the subject, knowledge about concussion still is inadequate in the general public.
Do you know that your child could still have a concussion without being knocked-out, unconscious or even “seeing shineys?” They can.
Do you know that a concussion can occur from a blow on the body nowhere near the head? It can.
The Center for Disease Control gives us this list:
Eight symptoms of brain injury seen in children with concussion
- Listlessness, tiring easily
- Irritability, crankiness
- Change in eating or sleeping patterns
- Change in the way they play
- Change in the way they perform or act at school
- Lack of interest in favorite toys
- Loss of new skills, such as toilet training
- Loss of balance, unsteady walking
In whatever sport or play activity a child participates, which gives a risk of concussion, vigilance must be given to watch for and identify these symptoms early so protection and treatment can be initiated.
While physicians may be in the best position to diagnose and make return-to-play decisions, they must rely on parents, teachers, coaches and other care-givers to notice these subtle changes that enable them to make those decisions.
11 Posts in Childhood Concussion (concussion) Series
- Helmits?! Do they prevent concussions? – 5 Apr 2017
- Video- concussion management – 30 May 2016
- Video: Concussion 101 – 6 May 2016
- TBI, concussion and early nutrition – 28 Apr 2016
- 5 things to know – 12 Sep 2015
- Football and brain damage – 21 Aug 2015
- 10 scary issues – 18 Jun 2015
- Reading test a predictor of concussion – 30 May 2014
- New guidelines for sports – 27 Jul 2013
- More dangerous than we thought – 24 Jul 2013
- Childhood Concussion Series: Intro/Index – 23 Jul 2013
Advertisement by Google
(sorry, only few pages have ads)