33 Things About Bugs A Doctor Needs To Remember
The last time I wrote about bug bites I told myself: “If I write one more thing about bugs, people will think I’ve got a fetish or something!”
Well I don’t, but here we go again! There’s just so many questions about them in people’s minds, doctor’s tend to forget about them compared to other daily crises, there’s a lot of articles still being written by others and… there’s just so many good photos lately.
Mosquito’s receptors target specific odors
More Bugs
and the problems they cause

I’m not the only one who’s heard “talking heads” on television predict that “when humans are long gone from the earth, bugs will still be here” or “bugs outnumber humans and if they wanted to they could take over the world!”
Those things sound stupid but somehow strikes enough of a chord in our minds that it provokes a twinge of worry—enough to believe they are true. Bugs aren’t the tiny, insignificant little things we pretend they are. Insects and arachnids emerge all over North America in the summer.
They roam our yards and homes looking for food and many times its… US! Thousands of species attack humans as either parasites or in defense and they can be both nuisances and deadly.
The “Kissing Bug” bites and leaves behind a swollen, itchy rash; but, also can leave Trypanosoma cruzi, the parasite causing the deadly Chagas disease (a bit rare in North America).
Let’s go through a list of the more common bugs and the thirty-three (or so) things that people commonly forget to consider about them. Take a crack at diagnosing them from the photos, if you can, before I tell you about them.
Red-based Pustules

This baby played outside on the deck for several hours yesterday and today you noticed these painful, itchy, red-based, swollen, pustules on her hands.
What do they look like to you? What “fiendish thingy” is most likely to have been feeding on your kid? A. Mosquitoes; B. Fleas (Pulex irritans); C. Bedbugs (Cimex lectularius); or D. Fire ants (Solenopsis invicta).
Fire Ants
I don’t think I’m the only one with memories of the coordinated way red ants attack all at once without warning. The “attack command,” whatever it is, seems to effect all of them at once and those who’ve been walking peacefully up your leg moments before turn vicious in unison.

Envenomation is painful in and of itself; but, many develop immunoglobulin E (IgE) reactions that can last 72 hours or more and even cause full-blown anaphylactic reactions which need to be treated with epinephrine every 10-15 minutes as needed to reverse symptoms.
Cool compresses and antihistamines are the mainstay of treatment. Topical steroid creams and in severe cases, oral prednisone might be needed.
Fire ants came from South America in the 1930’s. They are aggressive and outcompeted the local ants in North America, China, Australia and New Zealand. It was like what the killer bees would do years later.
Being so small (3-6mm) it’s easy for us to intrude on their territory and they are VERY difficult to eradicate. When not in defense-mode they readily eat organic garbage.
Fluid-filled Raised Rash

This little-older patient went outdoors too, hiking through the woods, and now has this rash on her arm.
It’s similar to the previous, but different. It’s raised and itchy and red; but, the redness is a bit more pronounced, the center a bit larger and is filled with fluid.
What does this sound like to you? It too is a bug bite; but which one is the most likely? A. Deer tick (Ixodes scapularis); B. Botfly (Dermatobia hominis); C. Chiggers (Trombicula alfreddugesi); or, D. Fleas (Pulex irritans)
Trombiculosis
If you diagnosed fleas I wouldn’t blame you a bit because I’ve seen a case just like this; but, it’s not, it’s Chiggers. And, frankly, in this photo it’s a bit more wide spread than I’ve seen Chigger bites and often you’re helped by seeing many bites in a single file because that’s how chigger larvae burrow and feed on skin cells.

Chigger (Trombicula alfreddugesi) larvae cause a rash known as Thrombiculosis as body tried to “fight off” the foreign substances that they inject into host cells which digest them until they burst and the mite can then easily suck up the nutritious juice.
Mite saliva causes intense irritation, with severe itching and dermatitis which can be helped a bit by over-the-counter topical corticosteroids and antihistamines; or, if necessary, more potent prescription medicines.
We don’t know chiggers to carry disease in the U.S. but in East Asia and Austronesia they carry a pathogen (Orientia tsutsugamushi) which transmits TsuTsugamushi [tsoo·tsoo·ga·moo·she] fever, a scrub typhus illness also known as Japanese river disease.
There also is something else going on with those bugs cause the Texan’s have analyzed chiggers in their state and found genetic material from the Hantavirus, and both Borrelia and Ehrlichia viruses inside them. Although, as I said, we have no known reports of those disease transmission to humans. How they got there and why they’re still there, we still don’t have a clue.
Petechial Rash On Arms and Joint Pain

Here’s another rash to look at. This one is on a 16-year-old Oklahoma boy who went camping last week and now got a low grade fever, a rash and his joints hurt when he moves.
The thing is, this kind of presentation of illness isn’t REALLY specific to any one disease BUT, believe it or not, the fact that he went camping in Oklahoma gives Oklahoma doctors a very high index of suspicion that it might be Rocky Mountain Spotted Fever (RMSF) [Yes, even though the Rocky Mountains are hundreds of miles away].
Rocky Mountain Spotted Fever (RMSF)
The thing is though, RMSF a tough disease to diagnosis for several reasons. The rash takes 3 days to up to a week to form and, no offense, a whole lot of patients these day don’t remember from one day to the next let alone last week. And even then may not even think camping is what you mean when you ask “have you been in the country or the woods lately.”

Seeing a rash like this on a patient who has had recent outdoor activity IS a major diagnostic sign of RMSF; BUT, 10-15% of patients never develop a rash AND it’s present in LESS THAN half by day three
And, geography also is key. Only five U.S. states account for over 60% of RMSF (North Carolina, Oklahoma, Arkansas, Tennessee, and Missouri) and they’re not even in the Rocky Mountains—and a huge number of them are in summer, peaking in June and July.
What I’m trying to convey is that doctors should NOT rely either on a patient telling them “I was outdoors and bitten by a tick” or even seeing the petechial rash in order to make the diagnosis.
Even with the diagnosis, treatment is a real trick too. We use Doxycycline for first-line treatment of both children and adults; but, it’s not the easiest on the stomach. We found tetracyclines mar developing teeth in children under 8 and chloramphenicol carries the risk of aplastic anemia even though it’s a good choice for pregnant patients.
If left untreated RMSF can become severe and even fatal; but, even in endemic areas, the treatment is so complicated that antibiotic prophylaxis after every tick bite is not currently recommended in the US.
You see, only some ticks are culprits. The American dog tick (Dermacentor variabilis) is the most common but it’s only east of the Rockies. The Rocky Mountain wood tick (Dermacentor andersoni) is in the Rockies and transmits both RMSF and Tularemia. And the brown dog tick (Rhipicephalus sanguineus) has been identified as a source of RMSF and is found a lot in the southwestern United States and along the US-Mexico border.
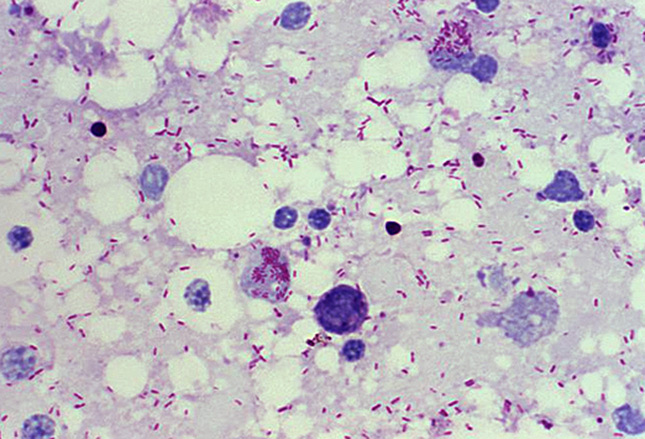
In addition, only SOME of these ticks are culprits, they have to be “sick” themselves. They have to be infected with the bacteria Rickettsia rickettsii like is shown in this photo—the tiny reddish dots.
The bacteria is hard to see and special stains are needed but you can see them on this tissue biopsy of the rash. They infect the cells which line the smallest of blood vessels and eventually cause them to leak blood cells out into the surrounding tissues&meash;which gives the rash in the skin and damage to organs and tissues.
“Target-shaped” Rash On Teen

This teen boy came with the odd rash in the photo as well as fever, headache and fatigue.
Can you guess which disease this rash is seen with? A – Tularemia; B – Ehrlichiosis; C – Lyme disease; or D – Colorado tick fever.
Lyme Disease
Similar to RMSF, Lyme Disease is also difficult to diagnose. Perhaps not when the patient is kind enough to come in with this rash, called a “Target Lesion,’ but less than twenty percent do.
The expanding red rash is called “erythema migrans,” is typically on the torso and sometimes multiple. Often it comes along with fever, headache and fatique—and perhaps, if we’re lucky, even a memory of the tick bite that did it to them.
Left untreated Lyme disease can spread to the joints, heart and nervous system; so, lucky for us, the disease does respond to a number of antibiotics depending on age, pregnancy and other considerations.
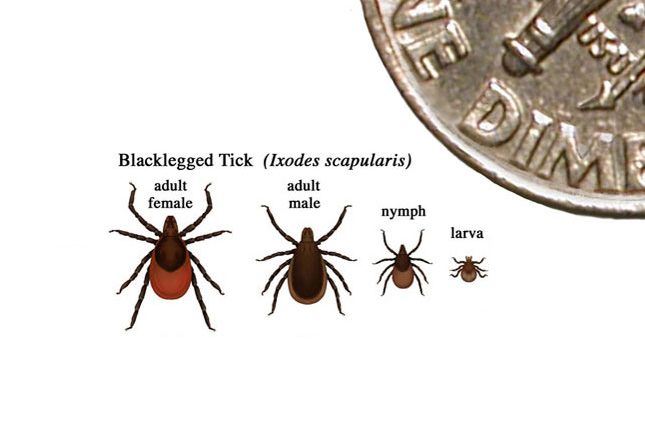
Also like RMSF, even though it’s mostly the black-legged, deer tick (Ixodes scapularis) which transmits the disease, only those which are “infected” themselves with a bacteria “Borrelia burgdorferi” give the disease to humans. Oops, I just remembered, in May of ’16 they discovered that “Borrelia mayonii” could do it too (if you’re keeping track).
But unlike the RMSF in most cases the tick must be attached for 36-48 hours (which they commonly are unless discovered) before the bacteria can be transmitted. That means that humans are most often infected by bites from immature ticks (called nymphs) which are less than 2 millimeters and very difficult to see. The adult ticks are most often noticed and removed before that.
Prevention
Those going into the woods in the summer, especially in the endemic areas shown on the graph, should wear light-colored, long sleeved clothing. Light-colored to make ticks easier to spot and long-sleeved to prevent them getting to you as much.
Permethrin can be applied to clothing as a repellant and can be used with DEET and picaridin over-the-counter repellants.
Ticks prefer warm, moist areas (eg, the beltline, groin, navel, and axilla) although the hairline is a common site for children.
Currently, no Lyme disease vaccines are available in the United States. (The manufacturer discontinued the Lyme disease vaccine LYMErix in 2002, citing low consumer demand.)
☤
As usual, I bit off more than I can chew in one bite and we’ve still got over half to go. Join me in part two for the conclusion.
7 Posts in Bug Bites (bugbites) Series
- Part 2 - 33 things about bug bites: fleas, bed bugs, spiders, Zika, Dengue and Ehrlichiosis. – 28 Mar 2018
- Part 1 - 33 things about bug bites: Ants, Chiggers, Ticks – 23 Mar 2018
- Ticks and Fleas – 11 Dec 2016
- Bed bugs, Mites and Lice – 7 Dec 2016
- Mosquitos and their illnesses – 23 Jun 2016
- Scabies is coming back! – 27 Oct 2014
- Bug Bites Series: Intro/Index – 15 Oct 2014
Advertisement by Google
(sorry, only few pages have ads)

