Poison Ivy, Oak and Sumac in Children
Ok, lets see how astute you are about summer medical problems in children.
You are the doctor and an adolescent comes into your office with swollen eyes and a rash over his face and arms with blisters which itch terribly.
You ask him the history and he says it began Wednesday after a camping trip Saturday and Sunday. He says it seems to spread and "itches like heck."
On physical examination you find pruritic patches of erythema, edema, papules, vesicles and bullae on his face, arms, chest, thighs and genitalia. Some in a linear distribution.
Translated that means you found areas of redness, swelling and raised rash with small and large blisters. Some of which would seem to be in a straight line.
 What is the diagnosis? Contact Dermatitis from a toxicodendron or Rhus antigen. In other words poison Ivy, Poison Oak, or Poison Sumac.
What is the diagnosis? Contact Dermatitis from a toxicodendron or Rhus antigen. In other words poison Ivy, Poison Oak, or Poison Sumac.
The rash is produced from coming in contact with an oleoresin (oil) found on the leaf, stem, branches, flowers, berries, seeds and roots of these plants.
It has been estimated that approximately 70% of people will develop a rash if briefly exposed to the oleoresin. Almost everyone would become sensitized if they receive prolonged exposure.
The first time you are exposed to the oleoresin the body is slow to respond – approximately 9 – 14 days.
However, subsequent exposures will produce the rash much more rapidly – 6 to 43 hours – depending upon the quantity of exposure and the persons sensitivity.
The first rash to appear is usually the area that was directly exposed to the plant.
But because the agent is an oil, the rash can occur from indirect exposure to contaminated clothing, pets, tools and hands.
The oleoresin on fingertips and under fingernails can "spread" the exposure to areas under clothing and the eyes.
treatment would be as follows:
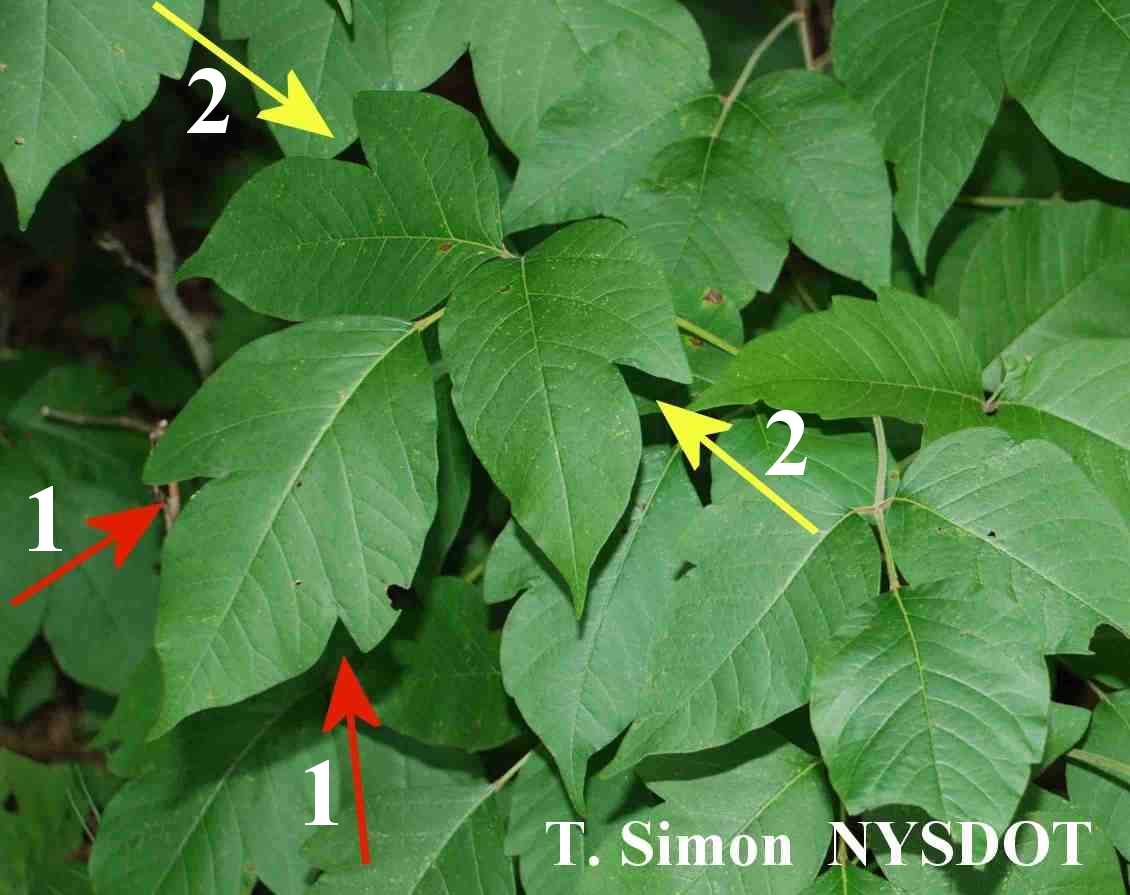
 Prevent exposure. Learn to recognize the plants and avoid them. "leaves three, let it be; berries white, run from sight."
Prevent exposure. Learn to recognize the plants and avoid them. "leaves three, let it be; berries white, run from sight."
Prevent rash from forming. Rash may be prevented by prompt removal of the oil with soap and water – within 10 minutes. But don’t rub it all around and spread it more.
Wash thoroughly. The area should be washed as soon as possible, including under fingernails, etc. to remove any unbound oleoresin which can remain potent for up to three days.
Prevent further contamination. Also important is that contaminated clothing and other articles should be washed as well, otherwise they can cause rashes for months.
Initial treatment. Small areas of rashes can frequently be controlled with cool compresses of water, salt water, or cold skim milk followed by calamine lotion.
Steroid cream. Try an over-the-counter (OTC) steroid cream first if the rash is on a fairly small area. If it covers a large area or if OTC medications don’t work, a steroid cream or spray will probably be recommended by your physician.
 Don’t use some types of medications. Preparations containing benzocaine, neomycin, antihistamines or zirconium should not be used because of their sensitizing capacity.
Don’t use some types of medications. Preparations containing benzocaine, neomycin, antihistamines or zirconium should not be used because of their sensitizing capacity.
Widespread rash. A rash covering more of the body may be helped by a colloid bath in addition to the above measures (Aveeno colloidal oatmeal or oatmeal and baking soda).
Itching. Itching can be helped by oral antihistamines (NOT topical) Benedryl or Vistaril.
Eyes and genitals. If the rash spreads into the eyes or on the genitalia or becomes infected it should be seen by your physician. On boys the penis may be the first area involved due to using the bushes to "go."
Very widespread involvement. Widespread involvement requires rest and oral steroids. Hospitalization may even be necessary for severe dermatitis.
Oral steroids. While they should NOT be routinely used in children, when other measures fail your doctor may give prednisone or its equivalent for approximately two to three weeks. The dose will be gradually tapered but if stopped too soon dermatitis usually flares again.
Watch for infection. If one of the lesions becomes infected with a yellow crusting, oozing and swollen lymph nodes your physician will give an oral antibiotic (not topical).
Cross reaction to other compounds. Individuals who are allergic to poison Ivy, Oak, and Sumac will also react to some lacquers, Cashew oil, Gingko fruit pulp, Black India marking ink and Mango rind, leaves and sap.
Advertisement by Google
(sorry, only few pages have ads)

