Parenting ADHD: Errors of commission and omission

Parenting ADHD Children
Parental errors of commission and omission
by Gregory A. Barrett, M.D.
One Problem, Many Names

A.D.H.D. can be a pretty confusing subject, beginning with just the name itself. It seems as though physicians and mental health professionals help make it that way by how they change its name every three or four years.
Originally the issue was known as simply hyperactivity, then it became minimal brain dysfunction, attention deficit hyperactivity disorder, attention deficit disorder, attention deficit disorder with hyperactivity, attention deficit disorder primarily inattentive sub-type, and on and on. (HK→MBD→ADHD→ADD→ADDHK→ADDi) Yikes! Enough already! For this discussion, let’s just delete all of those little periods between the letters, call it ADHD, and leave it at that!
An issue which disturbs both pediatricians and thoughtful parents alike is the amount of subjectivity (diagnosis by observational opinion) inherent in making this diagnosis. The field of psychology has been hard at work for years trying to quantify ADHD more scientifically; but, at its core, the labeling is dependent upon a variety of behavioral rating scales performed by parents and teachers – such as the Conner’s or the Vanderbilt.
Basically, these are tools used to quantify parents’, teachers’ and other caregivers’ observations and opinions about those children who have a combination of: 1) high activity level; 2) short attention span, distractibility, and difficulty concentrating; and 3) impulsivity – the lack of a pause between the thought and the action.
ADHD Parenting
 Hyperactives vs Inattentives
Hyperactives vs InattentivesThe two sub-types of this disorder are the “hyperactives,” – the classic male wall climbers who are easily identifiable by the classroom teacher within two weeks of the start of first grade; and, the infinitely more subtle “inattentives” – without hyperactivity who create no disturbance or disruption.
The latter just sit quietly in their seats paying no attention whatsoever to anything going on around them, chronically performing well-below their intellectual capacity, and remaining under the radar screen until someone says: “Hey, something isn’t adding up here.”
A bright child with this type of ADHD will often cruise through the early primary school years where the emphasis is more on understanding concepts. THEN, some will begin having noticeable difficulties when they hit fourth grade and their grades become based more on production; whereas, others may hit the wall upon entering the maelstrom of changing classes in middle school. At any rate, for many with this condition, there comes a time in the course of their education where they find themselves finally over-matched.
REAL Diagnosis of ADHD

There are four requirements which must be met prior to even considering any form of medical therapy.
First of all, they need to actually have ADHD, as documented by the behavioral rating scales previously mentioned. Fairly obvious, one would assume….
Secondly, the symptom complex must be present in both the home and school environments. If a child is inattentive, distractible, and unfocused in one arena, but not in the other, there is a high likelihood that a situational issue exists. It may be bullying, a student/teacher mismatch (all of us can recall a year like that, can’t we?), or a family conflict which is contributing to the symptoms. Alternatively, the diagnosis might simply be: being denied or not appreciated by either the parents or the classroom teacher.
Oftentimes parents will forward the argument that their son or daughter cannot have ADHD because they are capable of sitting still and playing video games for hours on end. Unfortunately, this observation proves absolutely nothing; because, in reality, sustained attention is not truly required in these games with their constantly changing fields and continuous stimulation.
In making this diagnosis the question is not whether the patient can watch cartoons for an entire afternoon without blinking; but rather, are they capable of harnessing their attention on demand, shutting out all other distractions, and focusing on the geography homework or book report uninterrupted for the next thirty minutes. This is the true challenge.
Similarly, a child may be underachieving but not causing any classroom disturbance and the teacher remains blissfully unaware of their problems with concentration. That happens, too. But for whatever reason [using proper pediatric practice] until both home and school are in agreement, it is improper to proceed further .

Thirdly, requirement number three is that the symptoms were recognizable prior to seven years of age. This is a very important and under-appreciated criterion which helps prevent physicians from falling into a diagnostic trap. ADHD is like eye color or blood type, in that: if you have it… in varying degrees, you will always have it.
Back in the 1970’s, when the diagnosis was first written about and medications initially prescribed, it was widely believed that when children reached the age of puberty the condition would be outgrown and there were no further benefits of treatment. No scientific evidence existed to support this contention; however, as the years went by further research clearly demonstrated that if an individual truly has ADHD, they have it for life.
Whenever a medical diagnosis is based on evidence as tenuous as behavioral rating scales there will always be an element of error inherent in the labeling; but, those who have biochemically based neurotransmitter deficient ADHD are lifers.
Now, as a person matures and increases their self-awareness, sophisticated compensatory techniques often develop which assist them in performing more than adequately without medication – i.e. developing an acute awareness of when attention begins to wander and knowing to take a break; but, it will always be there.
The takeaway point for the prescribing doctor is that no one suddenly “catches” ADHD on their thirty-sixth birthday. If the onset in a patient truly occurs beyond the early school years something else is happening in their life. It may be drug abuse, hyperthyroidism, grief, bipolar disorder, depression, whatever – but it is not ADHD. And these alternative diagnostic possibilities need to be evaluated thoroughly. Physician, beware!
Treat Only If Necessary
And lastly, and most importantly, if this complex of symptoms is verifiably: present at home and at school, has started at an early age, and is chronic in nature BUT does NOT lead to significant academic or social disability, then medical therapy is not necessary.
In other words, even if the child in question IS: unfocused, can’t sit still, and displays striking impulsivity; BUT, is getting excellent grades, has plenty of friends, stays out of trouble, and the teacher loves him; THEN, medication is not an appropriate consideration. It’s a pretty good practice in medicine (particularly when dealing with the set of drugs used in this diagnosis) never to treat just for the sake of treating.
Non-medicinal: Effective Intervention

There are any number of non-medicinal interventions (like individual tutoring) available for the child who fulfills the diagnostic criteria. Minor accommodations such as: seating in the classroom (front row with no chatty, distracting classmates nearby), homework logs, extra time allowance for test-taking, and many other subtleties an experienced teacher can initiate, are beneficial. And, of course, accessing all of the one-on-one tutoring that is available is extremely valuable.
Which Is Best
Although helpful, these behavioral therapies appear to be of somewhat limited value. The classic study which addressed this issue compared three interventions for children with ADHD — behavioral management, behavioral management plus medication, and medication without any psychological services.
The results indicated that both behavioral management plus medication and medication only were much, MUCH more effective than behavioral management alone. The unexpected finding was that the combination of medication plus behavioral therapies did not produce substantially better results in these kids than simply just taking the medication.
The takeaway point from these studies was the demonstration of the powerful role of the biochemical basis of this condition. Behavioral interventions will always be valuable adjuncts; but, generally speaking, in ADHD they are not adequate by themselves to produce the substantive change desired.
That by no means diminishes the importance of ongoing coaching to develop the life skills necessary to either: supplement the benefit derived from the medication; or, ideally, to be able ultimately to discontinue the treatment altogether. Teaching: insight, self-awareness and coping strategies, are crucial components of long-term management. However… medication does play a central role for many in getting to that point.
Non-medicinal: Ineffective to Fraudulent Intervention

Other non-medical interventions have been explored, but frankly as a group they range from ineffective to fraudulent. These fads all began with Dr. Feingold and his famous diet which started back in the seventies. Now the original Feingold diet was a far different beast than the later popular perception. HE suggested that avoidance of naturally occurring salicylates (aspirin-type chemicals in foods) – which were known to cause subtle allergic reactions or asthma in some sensitized people – might be beneficial in a sub-segment of children with ADHD.
When his diet was rigorously studied in strict clinical settings (repeatedly multiple times) it was unequivocally proven to be false; however, that didn’t prevent a small section of uninformed lay population from capitalizing on the fear-mongering idea that sugar in general and red food dyes in particular caused hyperactivity—another, rarely truly occurring phenomenon sometimes mistakenly blamed for nearly everything.
It is true that when one consumes a carbohydrate a biological reaction occurs: the level of blood sugar increases→the pancreas is immediately called upon to secrete insulin for the purpose of driving the sugar into the cells→and in some persons insulin overshoots the mark a bit causing hypoglycemia→which results in the release of epinephrine. This epinephrine can then give those children temporary symptoms of jitteriness and/or agitation until the blood sugar normalizes. However, any hyperactivity related to the physiologic response from a low blood sugar is short-lived and not sustained. And furthermore, when large groups of children whose parents swore sugar made them hyperactive were meticulously studied, no such effect was found.
The red dye theory also equally met its demise; so thoroughly that, after years of ignominious exile, the beloved little red M&M’s finally reappeared in the package. Uncountable numbers of megavitamin concoctions and other alternative therapies have not proven to be of any benefit, either.
Like it or not, the only dietary or medical treatments which have been scientifically proven to be effective are the ones physicians use to treat the issue!
Medication
How these medicines affect the brain is so simple it is almost ridiculous. First of all, one must understand the chemical basis of attention.
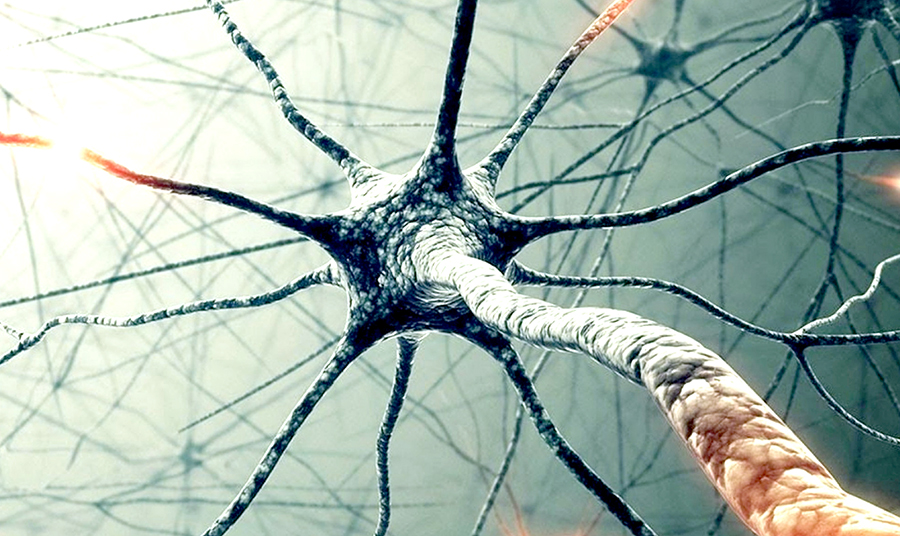
The example I like to use to explain this is the following: Picture yourself driving a car. Okay? Alright, now when are you most focused? That’s easy. You are most attentive when you hear the squeal of the brakes and the blare of the horn. At that point time slows down, you are not daydreaming or listening to the radio or distracted by anything else, you are focusing with one hundred percent of your mental capacity on the traffic situation at hand.
The reason why your concentration is so dramatically improved is that, in response to the classic fight or flight reaction, your adrenal gland has just pumped epinephrine (adrenaline) into your bloodstream – which is immediately broken down into norepinephrine and dopamine to act in the synapses, the space between your neurons (a.k.a. brain cells) – for the purpose of riveting your attention!
People with ADHD apparently just have a lower resting amount of these neurochemicals, leaving them attentionally challenged. Basically, the prescription drugs themselves are nothing more than stimulants which artificially increase the naturally occurring neurotransmitters back up to “normal” levels. (There is a newer agent, Straterra, which acts slightly differently in an attempt to create the same result. Unfortunately, in addition to taking four to six weeks to take effect it has proven to be much, much less likely than the stimulants to be beneficial. Straterra has its place, certainly, but for the sake of space and simplification I’ll leave that discussion for another time.)
Beyond Debate
One question that is beyond debate is whether or not these medications work. Any number of studies have shown that they are significantly and amazingly effective. And now that you understand how they operate, that result should not surprise you. Just think about yourself for a minute. Did all of those cups of coffee you imbibed late at night help you stay awake and concentrate better when studying for your finals back in college? Sure they did. How about drinking a Mountain Dew or a Red Bull during a break at the conference you attend? Wasn’t that a bit of a pick-me-up? Of course it was.

Well, Ritalin and its brethren work the same way. The dirty little secret is that everybody’s concentration improves somewhat from ingesting these pharmaceuticals, not just persons with ADHD. It’s just that anyone with big-time, chronic inattentiveness benefits to a far greater degree. And the need is much more compelling because of all the shortcomings and underachievement which result from a higher degree of distractibility.
The major issue with this class of drugs relates more to side effects than their safety. What is meant by that statement is that in spite of decades of shamefully widespread over-treatment, the safety profile remains remarkably good. The list of side effects, however, is lengthy including: increased blood pressure, increased heart rate, decreased appetite – especially for the lunch meal, initial weight loss, temporary slowing in linear growth, increase in muscle twitches or tics (debatable), mood changes, and difficulty sleeping. All of which physicians understand, watch for and have ways to mitigate.
However, the real-world perspective is that most children have none of the above side effects; or, if they do, they become quickly tolerant to the effects of the medication. The reactions diminish with time or alternatively disappear completely at a lower dose. And if they don’t, or the side effects are significant, the medication is simply discontinued or changed to an alternative.
The onset of response to the medication is nearly always immediate, the very first day. As with all treatments there is the placebo effect to consider; so it’s usually around a month or so into the trial before one can really determine the outcome to the initial dose prescribed. Therefore, neither the doctor nor the parents must allow themselves to become either too excited or conversely too disappointed prematurely.
If I have one strong bias in this regard it is that a successful trial should result in dramatic improvement with minimal, acceptable, or ideally no side effects. When a parent makes a statement such as: “Well, I don’t know, maybe he might be possibly just a slight bit better, I’m not really sure,” that is by my definition a treatment failure. If you’re going to be giving your child such a medication, there had better be a much more successful outcome than that. You want and deserve a lot more bang for the buck.
But don’t abandon ship too quickly, because another quirk of these medications is that the response curve is dose related. In other words, the higher the milligrams the more improvement one can expect to see. However, the greater the dose the greater the side effects, also. The target is that magical level of maximum benefit with minimum side-effects.
Teens

A crisis in therapy often occurs during adolescence. This is a most crucial period for effective treatment as: driving, substance use, and social interactions combined with unchecked impulsivity may have lifelong consequences. But ironically, it is at this very age that a patient will commonly become non-compliant with treatment!
There were many theories forwarded as to why this would be the case until investigators finally decided to ask the adolescents directly. And what the teens overwhelmingly reported was that they no longer wished to take the medication; not because they didn’t think it was helping, but rather because they didn’t like how it made them feel. And specifically, how they felt was “flat.”
These medications had, in some, the effect of narrowing their range of emotions; and the typical teenager, apparently, relishes the dramatic highs and lows of the age. Here is a critical time for “life-coaching” from a trusted adult.
Over-Diagnosed?
The primary issue of ADHD which makes all of us uncomfortable, me included, is the undeniable fact that this entity is obscenely over-diagnosed (even by physicians); which, I believe, is primarily due to the subjectivity inherent in the use of the behavioral rating forms.
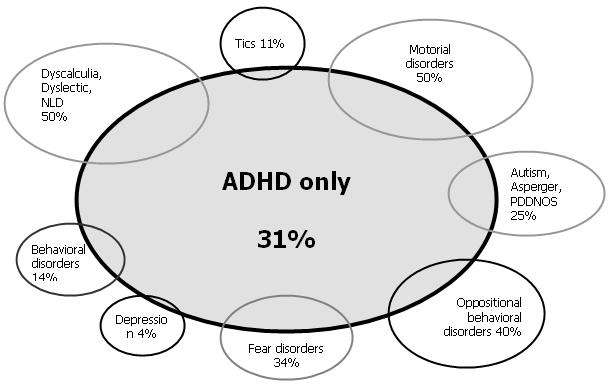
In addition there are the multiple alternative causes of inattention, as I mentioned before; including: lack of motivation, absence seizures, limited intelligence, mood disorders, and, of course, simple immaturity, among many others. (See the chart, click to enlarge)
Because of these overlapping entities, it is an unfortunate reality that there will always be an element of over-diagnosis inherent when dealing with ADHD.
However, although over-diagnosis is understandable, and to a certain degree acceptable, there is never an excuse for over-treatment. This is the key point. My prejudice, as previously discussed, is that there should be a rather spectacular clinical response to stimulant medication before considering the trial a success. That is how to stay out of trouble. And that is how one avoids over-prescribing these medications.
No reasonable parent really wants their child to be taking a chronic medication, especially one with potential side effects. And I guarantee the physician would rather not be playing a role in this, either. So, my philosophy is to set the bar extremely high. Many may qualify but few will be treated, at least long-term, if this approach is correctly applied.
One must acknowledge that there will forever remain an element of electivity inherent in the decision to treat. And it is a fact that some people with ADHD are living productive lives, at some level, without medication. This is largely accomplished in one of two ways, either: they select an occupation where the short attention span and distractibility are not handicapping; or they develop other effective coping strategies. But, there are also many others who continue to gain a lifetime of benefit from medical treatment.
Overwhelmed

Not infrequently parents come to my office with the complaint their child is struggling in school, and they express the desire to explore the possibility he or she may have ADHD. However, they want to make it clear right at the outset that they would NEVER consider the option of medication. Furthermore, this declaration is often made with a curious attitude of self-satisfaction; as if they were somehow morally superior to other parents whom they believe to be less caring or knowledgeable than themselves.
Well, the philosophy of wishing to avoid the use of drugs wherever possible is certainly commendable; but, why do they feel so strongly about this particular class of medicines? And shouldn’t they be consistent? If their child had recurrent, disabling seizures would they refuse anti-convulsants? If their child had cancer, would they be equally insistent about no chemotherapy? If their son or daughter had been diagnosed with diabetes, would they decline a prescription for insulin?
Actually, that is a rather appropriate parallel; because a child with true ADHD can no more concentrate and achieve their potential in the school setting without medication, than a diabetic can keep his or her blood sugar in the normal range by diet alone. No matter how much one yells or nags at such a child, and no matter how hard he or she tries, they are simply biochemically incapable of overcoming this condition on their own.
One might argue that these other conditions aren’t in the same ballpark as attention deficit because they are so much more severe. Seizures, cancer, and diabetes can be devastating, most certainly. But if one considers all of the proven consequences of untreated ADHD (recreational drug use, school failure, automobile accidents, low self-esteem, unplanned pregnancies, increased dropout rate, underemployment) the comparison isn’t quite as inappropriate as it seems on the surface.
Caution

I saw George Will (American political commentator) on television a few years back giving an editorial comment about ADHD. “These children don’t need a pill!” he practically spat at the camera, absolutely furious. In HIS opinion all they needed was a firm, masculine hand to guide them!
Well, I happen to have a great deal of respect for Mr. Will. I like him and much of the time I agree with him. And even when I don’t, I find him interesting and well-informed. I think he is a brilliant man and a wonderful writer, and I would never consider debating him on politics or baseball.
But when I heard him make those ill-informed, impassioned comments, I had to wonder to myself, “What in the heck does this guy know about pediatrics?”
Unfortunately Mr. Will, ADHD does exist. And like it or not, medication is often dramatically effective. As surely as chemotherapy destroys cancer cells and penicillin eradicates a strep infection, stimulant medication can help this subset of children.
Is attention deficit disorder over-diagnosed? It certainly is. Is medication over-prescribed? Absolutely! But mothers and fathers must not be afraid to look at their children with open eyes. Don’t be stubborn, and don’t pretend they are something they are not. Accept and consider the input of others who also care about your son’s or daughter’s well-being. And if you are a parent of such a child then it is your duty to carefully consider the pros and cons of treatment.
Don’t let your fear of commission (agreeing to a trial of medication), allow you to make a huge, and potentially life-altering, error of omission.
☤

