Adolescent Routine HIV Testing
The old adage “familiarity breeds contempt” is, perhaps, no more true than in the case of the AIDS epidemic. I call it an epidemic cause when 1.2 MILLION U.S. citizens are living with it daily (34 million world wide) I think it’s time to call a spade a spade. And that was in 2011, the last year we seem to have tallied the stats.
Transfusion related AIDS patient Ryan White and mother
The fact that we don’t seem to have our news “talking heads” blustering about it every night on TV apparently does NOT mean that AIDS has gone away or even gotten less severe; perhaps they just got tired of talking?
The leading healthcare advocate for children in the world, The American Academy of Pediatrics (AAP), encouraged HIV testing of all sexually active youth in a 2001 policy statement and that approach has had some effect.
However, HIV particularly affects adolescents and young people and they accounted for 39 percent of all new infections and 15 percent of all people living with HIV in 2012! It’s time for a re-think and an update – which has recently occured.
HIV: Current State of Affairs
So, here is a bullet list of the current facts before I get into the “why” and the latest recommendations and guidelines going forward:
- Most sexually active youth [65% of 12th graders by admission] do not feel that they are at risk of contracting HIV and have never been tested (<13%).
- The percentage of HIV/AIDS cases is increasing in the 15-24 age group.
- HIV in the top 10 leading causes of death in the 20-24 year age group.
- 55,320 U.S. HIV/AIDS cases (5%) are aged 13 to 24 years.
- Overall, 20% of the 1.1 million people with HIV/AIDS in the U.S. are unaware of their infection – who account for 54-70% of the new HIV infections. [Over a fourth of new cases spread from people who knew they had it!]
- 48% of HIV-infected adolescents and young adults were unaware of their infection.
- The risk of HIV infection varies with community prevalence rates, sexual behaviors, and concurrent substance use.
- In 13-24 age group, 73% of new diagnoses are male.
- For males, over two-thirds of transmissions are via male-to-male sex; females heterosexual.
- HIV occurs 7 TIMES more often in blacks and 2.6 times more often in latino than whites.
- Is more common in people living in the South and the Northeast.
- Drugs and alcohol use nearly assures risky sexual behavior.
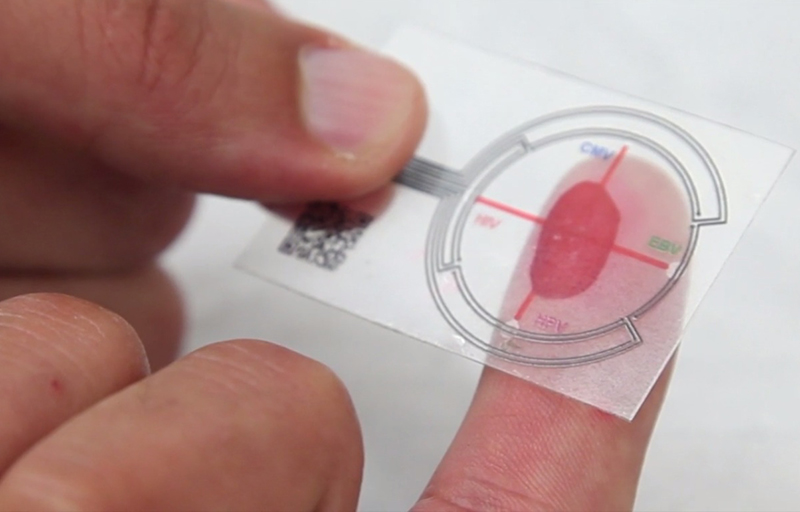
- Diagnostic testing has become easier and more widely available.
- Non-sexually transmitted HIV, while still present, has dramatically decreased due to vigilant blood product handling.
- A huge disparity exists between “developed” and undeveloped countries; and between races in developed countries.
AIDS Initiatives: What’s Gone Wrong?
The HIV virus has been around and even reached the critical mass to make the press several DECADES ago now! Comparatively, we hear little about it any more but the bullet points show that we’ve made little headway in preventing a disease which is so both deadly and debilitating. Why?
For one thing, this issue is nearly all about SEX. A mostly taboo subject in polite conversation. Not only that, in developed countries statistics show that it’s mostly about GAY SEX – a subject which has become so in-your-face yet politically incorrect to disparage that the media lives in fear of publishing anything that might be taken as derogatory in the slightest.
Secondly, the disproportionately larger HIV increase in children and young adults is exacerbated by the secrecy behind the whole sexual acting out thing. They don’t willingly want to reveal their behavior to anyone with the ability to help them – even doctors, although we’ve usually got it better than parents (if we can get them to come in.)
Thirdly, all prevention efforts to date against HIV have used “for cause” targeting, i.e. in “at risk” or “sexually active” populations. So, if there’s a cloud of secrecy and denial and parents don’t have a clue what chance does an outsider have in choosing who to target limited resources at?
It takes time and a great amount of effort on the part of “helpers” to gain the trust of and valence in the eyes of young people necessary to make a difference in their lives on anything, let alone issues of sex.
The only thing we have are generalities and statistics to focus our efforts so that’s what we must use if we ever hope to get ahead of this thing.
New Recommendations Going Forward
A frustrated Center For Disease Control (CDC) came out with their new recommendations some months ago, the AAP fairly recently, and both vary only a little.
The CDC Approach
The CDC seems to reason that if targeted testing and counseling isn’t working then we should take the bull by the horns and test everyone in the age group – at least once and those more at risk (sexually active or drug users) more often.
HIV screening has now been changed from only known sexually active populations to universal screening.
The CDC guideline: “All patients aged 13 to 64 years who are seen in health care settings should be tested for HIV in an “opt-out” basis” – i.e. you get it without asking or signing anything unless you specifically decline it.
In reported efforts, using that method, “over 50% of youth were offered HIV testing, and only 13% opted out.” [No wonder, even if the so-called “offer” wasn’t hidden in mounds of paperwork how would a teen refuse if his parents were there?]
They do include the caveat “unless or until the HIV prevalence rate is less than 0.1% of the community.” And, it’s not their job to generate the legalities necessary to circumvent the minefield the bureaucrats have created surrounding confidentiality, disclosure, and consent for caregivers of children and teens. They’re just expecting the various states to bring their laws into compliance with the guidelines.
Also in full disclosure, the idea of “prevalence rate less than 0.1%” is at best difficult and at worse impossible to ascertain for any one physician or community. First, the only prevalence statistics published are from 2011! Secondly, statistical breakdowns by “community” are pretty much non-existent.
Using the prevalence data currently available from the CDC, let’s take a look at what the screening means in some aspects:
At the national level, basically every race except Asians have prevalence rates over the desired 0.1% threshold.
At the state level, blacks meet the criterion for testing in every state – in Utah by 9 times, in the US overall by 12 times and in Washington DC by 44 times! Latino’s meet the testing requirement in every state but Idaho, Montana and North Dakota.
Whites should be tested in every state except 17 of them; although in many only avoiding the threshold by miniscule amounts. Asians would only be screened in Washington DC, Nevada, New York and Rhode Island.
Seems a bit difficult to manage screening exceptions to me; but that may be the CDC’s intent – to provide a goal to shoot for.
So, with such a huge difference in prevalence by race, do we screen by prevalence data lumped by state or
AAP Recommendations
- Routine HIV screening should be offered to all adolescents at least once by 16 to 18 years of age in health care settings when the prevalence of HIV in the patient population is more than 0.1%.
- In areas of lower community HIV prevalence, routine HIV testing is encouraged for all sexually active adolescents and those with other risk factors for HIV (eg, substance use).
- High-risk youth should be tested annually for HIV. Adolescents tested for other STIs should be tested for HIV at the same visit.
- Emergency departments and urgent care facilities in high-prevalence areas should implement routine HIV testing, which will provide an excellent opportunity to reach youth who do not seek primary care services often.
- Physicians should recognize the symptoms of the acute retroviral syndrome, such as mononucleosis-like syndromes, and consider including HIV RNA testing (viral load) in the diagnostic workup of youth when the appropriate risk factors are present.
- Although parental involvement in adolescent health care is always desirable, consent of the adolescent should be sufficient to provide testing and treatment for HIV infection or STIs. Pediatricians should make use of free and confidential community-based testing programs if there are cost or confidentiality concerns.
- Pediatricians should assess sexual and substance use behaviors, an essential component of routine adolescent care, regardless of perceived risk. Standardized assessment tools and a confidentiality protocol can be helpful.
- Pediatricians are encouraged to create an environment of tolerance and facilitate open discussion of gender and sexual orientation.
- Opt-out HIV testing is preferred if allowed by state laws, and rapid HIV testing has similar sensitivity to EIAs and can provide immediate notification of preliminary results. Physicians must follow the guidelines of their local jurisdictions for routine HIV opt-out testing in adolescents and are encouraged to advocate for change when such jurisdictions create barriers for implementation of opt-out testing.
- A negative HIV test result should be used as an opportunity to counsel adolescents on sexual and drug use behaviors to reduce future risk.
- For adolescents with a positive HIV test result, it is critical to arrange linkages to age-appropriate HIV specialty care, including prenatal care when appropriate.
- Pediatricians are encouraged to advocate for the dissemination of accurate, evidence-based prevention education, access to confidential HIV and STI testing and counseling, and HIV treatment for adolescents.
- Preventive care screening should include universal coverage and adequate payment for HIV testing and related counseling. Physicians should advocate for confidential billing practices related to HIV and STI testing in adolescent and young adults.
[http://pediatrics.aappublications.org/content/128/5/1023.full.pdf+html]