Breastfeeding and Human Milk
One of the most common topics for medical articles these days (besides immunizations) is breast feeding. There’s really a lot of them. It’s almost like people are trying to make a point.
Infant breastfeeding
And many of them seem to be written in the tone of trying to convince everyone that it’s a good thing to do. Truly, I’m not sure who it is that needs to be convinced.
I’ve been filing these findings in a box thinking some day I’ll do an article on them and the box is now quite stuffed. So, today’s the day. The problem is that most of them are quite esoteric and lengthy – won’t do at all for a blog article.
In this, the first of two articles, I’ll basically headline each research finding and then attempt to synthesize in “regular” language what it means. The next article will pretty much be a table of all the several new “official” recommendations for effective breast feeding.
Breastfeeding V. Bottle Feeding
From an “ol’ codgers” perspective, there used to be a whole lot more breastfeeding going on – with a whole lot less drama – than there is now.
Don’t get me wrong, the invention and continued improvement of infant formulas was truly a godsend for many mothers and their infants – and still is. Back then, however, the norm was to breast feed and I had distraught mothers in the office thinking they were failures if they needed to use formula. They needed information to be able to defend themselves, if only in their own minds, that formulas were still adequate nutrition and their babies weren’t going to suffer.
I’m not sure when the proportions began to flip on their head, perhaps about the timeframe we used to call “women’s lib”; but, without fanfare, gradually formulas became more advertised, “enhanced and improved,” and more commonly used. Definitely more convenient for working mothers – and absent any evidence to the contrary – there was nothing to prevent the “media blitz” from having it’s intended effect.
Now that the pendulum has swung far in the opposite direction there is enough experience to make the necessary statistics show up; so, let’s list a summary of those research studies which show significance.
Current Research Findings
Respiratory Tract Infections and Otitis Media
 Mother comfortably breastfeedingThe findings of three separate studies I’ll mention. First, any breastfeeding at all reduced the incidence of otitis media (ear infections) by 23% over those fed commercial infant formula – but is it the formula, the nipple, the bottle… who can tell? Exclusive breastfeeding for more than 3 months reduced it by 50% and if for 6 months, serious colds, ear and throat infections dropped 63%.
Mother comfortably breastfeedingThe findings of three separate studies I’ll mention. First, any breastfeeding at all reduced the incidence of otitis media (ear infections) by 23% over those fed commercial infant formula – but is it the formula, the nipple, the bottle… who can tell? Exclusive breastfeeding for more than 3 months reduced it by 50% and if for 6 months, serious colds, ear and throat infections dropped 63%.
Secondly, another study revealed that exclusive breastfeeding for more than 4 months reduced hospitalization for pneumonia by 72% in the first year of life. Additionally, even babies breastfed for 4-6 months still had a four-fold risk of pneumonia compared to those exclusively fed longer than 6 months.
And third, hospital duration and oxygen need of babies with Respiratory Syncytial Virus (RSV) is reduced by 74% in exclusively breastfed infants for 4 months compared with never or partially breastfed.
Gastrointestinal Tract Infections
Nonspecific vomiting and diarrhea infections seem to drop by 64% if a mother breastfeeds her infant in any amount; which reduction lasts for 2 months after cessation of breastfeeding.
Necrotizing Enterocolitis
Infants born preterm cannot yet nurse strongly so must be supplemented in some way – sometimes making it a real circus trying to induce and maintain lactation in order to obtain mother’s milk saans the baby. Back in the late 1900’s we discovered that the destructive bowel problem premature babies had wasn’t just from being premature – it was from the cows-milk formula used as a supplement. Prematures were then saved from Necrotizing Enterocolitis (NEC) by exclusively using mothers milk instead of cow’s formula.
These days, without the historical threat of imminent demise, sometimes there is even the understandable (but illogical) desire to avoid using a wet nurse. I guess that’s what prompted a recent study trying to sneak back in a little supplement with cow-milk-based formula – not, as it was proven, such a good idea. Preme infants fed exclusively human milk had 77% less NEC than those supplemented even just a little bit.
Sudden Infant Death Syndrome (SIDS) and Infant Mortality
SIDS is known to have so many other causes that having confidence in any statistics is difficult. There are significant numbers of SIDS cases in those exclusively breastfed; however, even when subtracting out for other causes, we saw an increase in SIDS as infant formula use increased – so something was afoot.
Ninety percent of world SIDS deaths occur in the 42 developing countries. In their circumstances exclusive breastfeeding for 6 months and weaning after 1 year is the most effective intervention a mother has! Extrapolating from those statistics, breastfeeding has the potential of preventing over a million infant deaths per year! Equal to preventing 13% of the world’s childhood mortality!
 Premature infant recovering from NECExclusive breastfeeding does seem to be associated with a 36% reduced risk of SIDS – even confirmed to be independent of sleep position. The smaller portion of world SIDS deaths which occur in the US is still a sizeable number. The calculation is that more than 900 infant lives would be saved in the US if 90% of mothers merely exclusively breastfed for 6 months.
Premature infant recovering from NECExclusive breastfeeding does seem to be associated with a 36% reduced risk of SIDS – even confirmed to be independent of sleep position. The smaller portion of world SIDS deaths which occur in the US is still a sizeable number. The calculation is that more than 900 infant lives would be saved in the US if 90% of mothers merely exclusively breastfed for 6 months.
Allergic Disease
Just how much exclusive breastfeeding has slipped in the US is highlighted in the research about allergic disease. Such a low prevalence of breastfeeding renders studies on the timing of additional solid foods less meaningful for breastfed infants.
There is a protective effect of exclusive breastfeeding for 3-4 months. It reduces the incidence of clinical asthma, atopic dermatitis and eczema by 27% in the low-risk population of infants and up to 42% in infants with a positive family history of atopy.
There is no solid evidence about the timing of adding solid foods except to say don’t do it before 4 months of age. The research about any other time-line is so conflicting (2015) that any advice must be considered “best guess.” The same can be said about any advice regarding delaying potentially allergenic foods after 6 months.
Celiac Disease
An unexpected (at least to me) odd finding is that there is a 52% risk reduction of developing celiac disease IF the infant is introduced to gluten (think wheat) while they are being exclusively breast fed.
There is an overall inverse association between the length of time being breastfed and the development of celiac antibodies. So, the factor isn’t so much the timing of the initial gluten exposure but the overlap of breastfeeding at the time.
Therefore, gluten-containing foods (bread, cereal, crackers etc.) should be introduced while the infant is receiving only breast milk and not formula or other milk products.
Inflammatory Bowel Disease
This one is a significant statistical relation only; because, we don’t understand all the possible confounding factors. Breastfeeding leads to a 31% lower risk of developing inflammatory bowel disease in later life.
We see it, it’s there; but, we can only hypothesize that it results from the interaction of the immune effects of human milk and the underlying genetic susceptibility of the infant. However, there might also be additional benefit related to different patterns of intestinal bacterial colonization between breastfed and formula–fed infants.
Obesity
 Oh, I wish we actually understood even half of what we know about obesity! In the case of breastfeeding there are still huge unknowns. Is it: Human milk vs formula or breast vs bottle? Or, something else entirely.
Oh, I wish we actually understood even half of what we know about obesity! In the case of breastfeeding there are still huge unknowns. Is it: Human milk vs formula or breast vs bottle? Or, something else entirely.
Known: Rates of obesity are significantly lower in breastfed infants – for whatever reason.
Known: Obesity campaigns which begin with breastfeeding do better than those which don’t.
Known: ANY breastfeeding yields a 15% to 30% reduction in adolescent and adult obesity rates.
Known: Massive studies show lower BMI and higher high-density lipoproteins in adults who were breastfed infants.
Known: Breastfed siblings weigh 14 pounds less and are less likely to reach BMI thresholds for obesity than their formula-fed brother or sister.
Known: Each month of exclusive breastfeeding gives an additional 4% reduction in risk of being overweight.
Some of these “knowns” would be “better known” if the many large-scale studies had thought to gather the data of whether it was “formula” in the bottle or “human milk” that was in there. Why? Because we also know that:
Known: Breastfed infants self-regulate their own volume consumed no matter how much the mother takes measures to make more milk available in the breast.
Known: Early programming of self-regulation in an infant affects adult weight gain.
Known: Infants fed by bottle, whether formula or expressed breast milk, have increased bottle emptying, poorer self-regulation and excessive weight gain in late infancy (> 6 months) compared to breastfed infants.
Diabetes
The incidence of type 1 Diabetes Mellitus (mostly children) in the general population is well known. Looking deeper however, more type 1 diabetics were formula-fed than breastfed. Exclusive breastfeeding for 3 months is shown to give a 30% reduction in the incidence.
It may be due to the avoidance of cow milk β-lactoglobulin which has been shown to stimulate an immune-mediated process that cross-reacts with the body’s pancreatic β cells.
The incidence of type 2 diabetes Mellitus (related to weight) is also reduced 40% in adults who were breastfed as infants, and the informed guess here is the long-term effect of breastfeeding on weight control that was mentioned above.
Childhood Leukemia and Lymphoma
There is a reduction of 20% in the risk of acute lymphocytic leukemia (ALL) and 15% in acute myeloid leukemia (AML) for infants breastfed for 6 months or longer. Those numbers drop to 12% and 10% if the infant is breastfed less than that.
The statistic is real but we’re trying to figure out whether it’s due to a direct protective effect of human milk OR is mediated by the reduction of early childhood infections.
Neurodevelopmental Outcomes
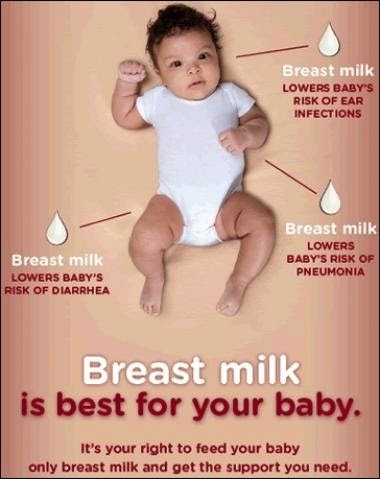
 Ad campaign poster for breastfeedingThese statistics are a bit more “grey area” than those I’ve covered above but are consistent across several studies. There are differences in the neurodevelopment of breastfed and formula-fed infants. It’s just that there are so many confounding factors studies have to deal with like parental education, intelligence, home environment and socioeconomic status.
Ad campaign poster for breastfeedingThese statistics are a bit more “grey area” than those I’ve covered above but are consistent across several studies. There are differences in the neurodevelopment of breastfed and formula-fed infants. It’s just that there are so many confounding factors studies have to deal with like parental education, intelligence, home environment and socioeconomic status.
At least one large, randomized breastfeeding intervention trial gave evidence that intelligence scores and teacher’s ratings (adjusted for confounding factors) are significantly greater in breastfed infants than formula-fed.
Both intelligence scores (on standardized tests) and teacher ratings (also standardized) are higher in those infants exclusively breastfed for 3 or more months. This observation is much more pronounced for preterm infants who are obviously at higher risk for neurodevelopmental problems.
Preterm Infants
The early discovery of an association with infant formula to NEC (above) prompted much more research about human milk use in the newborn intensive care unit (NICU). Both short- and long-term benefits have been found.
Using human milk for premature infants is shown to lower rates of sepsis and NEC. Additionally, there are fewer re-hospitalizations in the year following discharge from the NICU. There are lower long-term growth failures. There are less neurodevelopmental disabilities. Feeding tolerance is improved. Attainment of full enteral (by mouth) feeding is hastened. All by a diet of human milk!
NICU “graduates” who received human milk had higher intelligence test results and more “white matter” plus brain volume on imaging tests at 8 years of age through adolescence; also less retinopathy.
Studies done on extremely preterm infants, who therefore received the greatest proportion of human milk, had significantly greater scores for mental, motor, and behavior ratings at ages 18 months and 30 months – even after adjusting for factors like maternal age, education, marital status, race and other associated morbidities.
Breastmilk-fed pre-term infants also show lower rates of metabolic syndrome (problems of obesity) through their lives. In adolescence there is lower blood pressure and low-density lipoprotein [LDL (bad) cholesterol] as well as improved leptin and insulin metabolism.
Summary
 This may be quite enough to be going on with. What do you think?
This may be quite enough to be going on with. What do you think?
I’ve presented a whole lot of research here, how do YOU put this all together? To be honest, reading each of the individual research articles is innocuous enough; but, compiling them together seems like something must be just a tad bit exaggerated. Like it was if you had a choice: your baby could either be breastfed or be from Krypton, it would be the same.
It just seems a bit arrogant to me for mere mortals to be making the statement; but, I guess these days it does need to be in writing: “Breast is best.”
We simply must keep in mind, and take into consideration, that there are several contraindications to breast feeding, i.e. when it isn’t in the best interest of the infant to breast feed. There are some times when the baby’s own mother shouldn’t be the milk provider and some times when it just isn’t possible to breastfeed.
Recognizing that, the AAP has always tried to word official recommendations carefully so as not to burden an already stressed situation; and they continue to do so. The facts speak for themselves and it’s fair that everyone knows them.
We’ll take up what “officials” have made of all this research and what their recommendations are in the next article. For now let me leave you with one of the more succinct versions of the many position papers published by organizations charged with improving the world’s children’s health.
Breastfeeding and human milk are the normative standards for infant feeding and nutrition. Given the documented short- and long-term medical and neurodevelopmental advantages of breastfeeding, infant nutrition should be considered a public health issue and not only a lifestyle choice. The American Academy of Pediatrics reaffirms its recommendation of exclusive breastfeeding for about 6 months, followed by continued breastfeeding as complementary foods are introduced, with continuation of breastfeeding for 1 year or longer as mutually desired by mother and infant. (AAP position paper, )
[American Academy of Pediatrics and US Department of Health and Human Services – position paper publications]
4 Posts in Breastfeeding (breastfeeding) Series
- Recommendations and standards – 24 Mar 2015
- Research findings – 16 Mar 2015
- OBGYN Guidelines about breastfeeding – 26 Feb 2014
- Breastfeeding Series: Intro/Index – 20 Feb 2014

