Common Foreign Bodies Found In Children and Teens
The featured photo is not quite what I mean by the title of this post – it says: foreign bodies found “In” children, not “On” children. Oh well.
I have taken probably more foreign objects out of people than the average pediatrician in my career. Mostly because our Naval base hospital didn’t actually have “pediatric” gastroenterology, otolaryngology or respiratory services to rotate through in our residency so went through the adult services and saw all commers– and believe me, people do the “darndest things.”
“Foreign body” ON a boys nose
Foreign Bodies and Children
While infants and toddlers’ favor their mouths (and lungs), and preschoolers seem to favor their noses, teens and young adults… well, let’s say… explore orifices they haven’t tried before.
GI Tract
Every parent knows the danger of leaving any small object around the house when there is a child about; even if they don’t always remember to do it. When we forget, the built in “foreign object finder” we’ve given birth to often has a dramatic method of reminding us.
A day doesn’t go by in any emergency department (ED) without removing something from someone’s ear, nose, airway, rectum, vagina, eye or gastrointestinal (GI) tract. And each “something” and each “orifice” carries with it it’s own unique problem, difficulty and technique.
Smart physicians always keep a healthy suspicion that any odd sounding complaint might be a foreign object hiding somewhere where the patient is either too young to know, or to embarrassed to tell you.
Esophagus – Radiopaque
The hunting expedition begins with an x-ray study. But only certain solid objects show up on film (i.e. radiopaque) such as the coin in the stomach on the left and the “kitty” in the esophagus on the right.
“Swallowings” are usually accidental in adults and they show up in the office fairly quickly afterward. Children on the other hand usually don’t show up until there is some complication, which may be days later with a very confusing history. An object in the esophagus might produce weight loss, drooling, vomiting, chest pain, sore throat,
Esophagus – Radiolucent
Some objects like plastic, wood or even aluminum don’t show up on x-ray (i.e. radiolucent) so diagnosis must be made by using the “back-door” approach. A small amount of “contrast” is introduced to see if there’s a deviation or “filling defect” outlined by the contrast – like the plastic beads in the child’s esophagus to the left. Sometimes we even use “metal detectors” to help us decide if a swallowed object is “up top” or has passed “down below.”
Fortunately for all of us, most objects do pass harmlessly through the GI tract; unless, of course, they’ve got sharp angles or are too large in some dimension to make it past one “bend” or another. Some have toxicity to be considered and lacerations or tearing must be thought of; both by the object itself and the methods used to try to extract it.
Obviously, those complications must be resolved by endoscopy or an “otomy” (cutting open) of some kind, like a thoracotomy for a torn esophagus.
Intestines – Passing Through
This “passing through” thing – what is we need to do and how do we know when it’s done it? There are some “rules of thumb” we use to manage such things.
The esophagus moves so quickly and spontaneously that if we see any object still in the esophagus when we take an x-ray, we consider it impacted and that it needs to be manually removed. We do NOT use manipulation or Ipecac to induce vomiting.
Below the esophagus, blunt objects ingested within the last 24 hours often are “watched” for awhile; because, they usually “pass” on their own. Daily x-rays are used to watch them pass through and parents are instructed to catch and check all stools until the object is found.
Very sharp or pointed objects (i.e. sewing needles) on the other hand may perforate the intestinal wall and we remove them quickly using an endoscope.
Intestines – Long or Wide
From the stomach there is a narrow passage called the pyloric sphincter. A swallowed object in the stomach might be too long (greater than 6 centimeters) or too wide (greater than 2 centimeters) to make it through and must be removed.
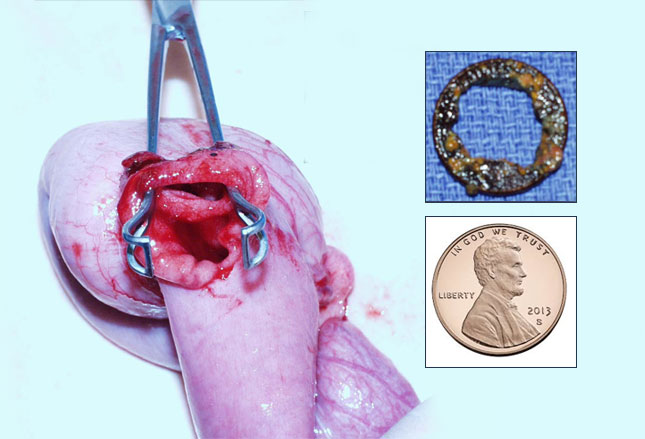
Additionally, any congenital or post surgical narrowing of the GI tract is a risk for impaction and must be followed closely by some means. The photo is part of a child’s small bowel which needed to be removed because of a penny which got stuck behind an unsuspected intestinal web.
They found the jejunum to be dilated and the penny partially eroded; however, luckily this was high up in the intestine enough that it could be reached with an endoscope. Lower down in the intestine objects need to be removed by surgery.
While they’re inside, foreign object start produce inflammation which then leads to pain, bleeding, scaring, obstruction and/or perforation.
Rectum
Once a foreign object has made it all the way down to the colon it usually has no trouble passing out the rectum, but on rare occasion they don’t.
And now that almost no one uses rectal thermometers any more, it is rare that anything except perhaps a suppository should be placed in a child’s rectum. If something is found either abuse or some psychological issue is considered.
Older teens and adults, on the other hand, are seen in the ED with rectal foreign objects more often than you’d realize (or perhaps approve of); usually the result of sexual activity.
Often the most damage is seen as the result of attempts to extract it prior to coming to the doctor. X-rays are done to certify the type of object isn’t fragile and breakable before attempts at extraction are made. Evidence of “free air” or fluid inside the body means that the object has likely perforated the bowel wall.
Intentional Body Packing
To avoid detection by the police sometimes teens might swallow hastily wrapped bundles of illicit drugs. On other occasions, bundles of drugs packed in balloons or condoms may be intentionally swallowed for smuggling purposes. Or inserted into the rectum or vagina.
Both of these procedures are incredibly dangerous (and stupid) from a medical standpoint almost always producing death or severe impairment from a massive overdose should any of the capsules break.
To complicate the problem, not infrequently the “packets” rupture when any attempt is made to remove them.
Urethra
Similar to the rectum, foreign objects found in the urethra of children usually require more intervention than mere removal. Because of mere location in boys there may be some personal exploration but the tenderness usually prevents insertion of anything.
Insertion of anything except carefully designed and manufactured objects such as catheters or endoscopes nearly always produces trauma and scaring as well as introduces infections.
On occasion, an object inserted into the urethra will slip fully into the bladder which will certainly require surgical removal. The urethra is particularly prone to develop subsequent strictures, fistulas and obstructions once it has been manipulated.
Ear
Next to the nose, ears are the most common “hiding place” for foreign objects in children. Food, toys, beads, stones, insects, seeds—if they fit, we’ve seen them in a child’s ear.
If they are too young or afraid to communicate that something is in their ear, we usually find them “by surprise” when we are examining them for pain, discharge, hearing loss or “fullness.” The longer they’re there, the more damage and the more symptoms.
Bugs or hearing aid components are the most common in adults. Luckily items lodge within the outer canal; if the item is in the middle ear, it means it must have punctured the ear drum. If it’s in the inner ear… well, it doesn’t get there without permanent damage to the hearing or deafness.
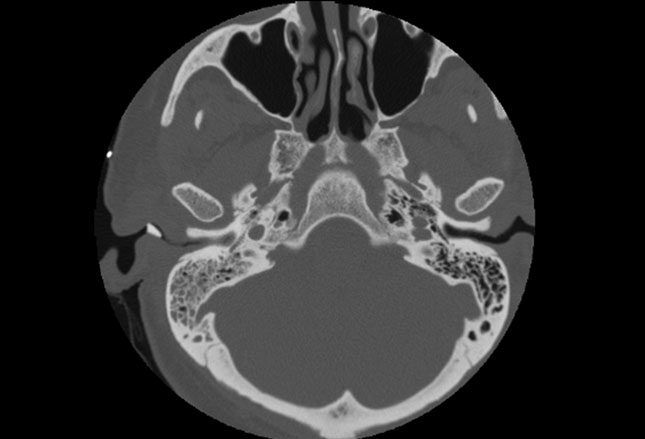
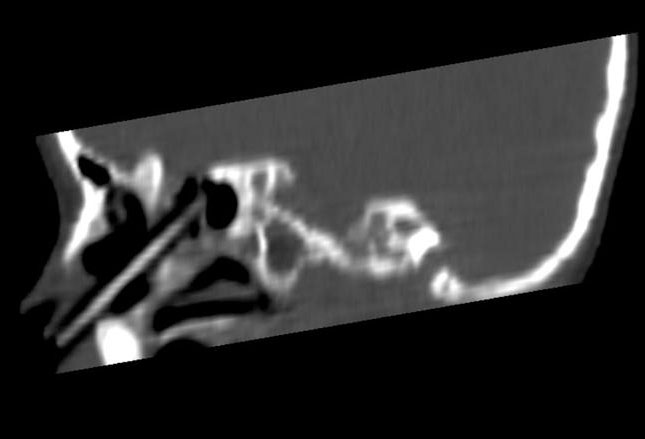
The computed tomography (CT) scan shows a metallic foreign body in the right external auditory canal.
Ear
Unless you work in the industry there really is nothing you have at home which can remove a foreign object from an ear canal (not even Q-tips) and it may make matters worse if you try.
Simple short tweezers might grab onto something IF you can see it and know that it won’t damage anything on the way out! Otherwise, just get into urgent care where they can remove it in safety.
We have several methods that we use, but all of them can do damage without an experienced hand. Low pressure irrigation can be used IF the ear drum hasn’t already been punctured OR is organic in nature (due to swelling with hydration).
We have tiny little forceps and hooks we can grab with but some magnification is usually needed to prevent pushing things in even further or doing damage in extraction. Suction too can be used BUT obviously that can suck out more things than the object if you’re not careful.
Nose
By far and away the most common repository for foreign objects, especially in boys, is their nose. Children’s anatomy make these particularly at risk of becoming dislodged into their airway—which will then mean real trouble.
Synthetic beads and vegetables lead the list of “insertables” but anything small enough is game. Things get stuffed into the right nostril twice as often as the left and I’ll let you guess why.
This is so common that if you ever see a child with a runny nose only on one side, just bundle them into the car and head to the doctors! Other signs and symptoms of something in the nose are: nasal irritation, bloody nose, sneezing, snoring, sinusitis, stridor, wheezing, fever, and halitosis.
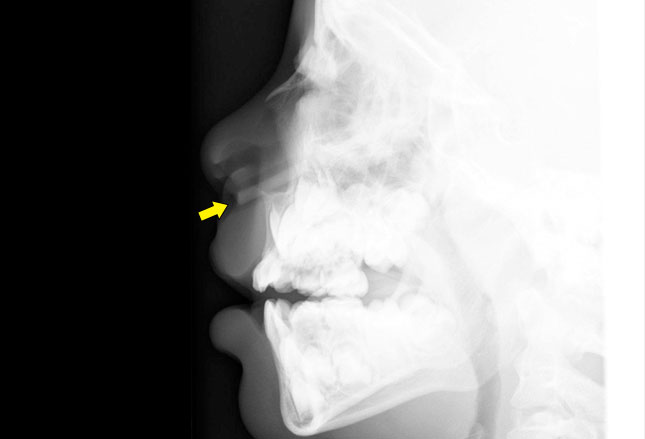
The x-ray shows the white shadow of a linear object in the nasal cavity (arrow) which appears to reach clear back to the sphenoid sinus (straw? crayon? carrot?).
Nose – Crayons, Buttons, Batteries
Not only is the nose a dangerous passage into the lungs for foreign objects, it has highly vascular tissue, lots of bumpy ridges and openings into all the major sinuses of the skull as well as the middle ear!
Any object causes mucous production as well as inflammation and infection. Once that happens significant side-problems like sinusitis develop which may be very difficult to treat even after the object is recognized and removed.
Metallic button batteries are of extra concern, because they cause low-voltage electrical currents, electrolysis-induced release of sodium hydroxide and chlorine gas which destroys tissues—within 12 hours. And that’s not counting the liquefaction necrosis if their alkaline contents leak into the surrounding tissue!
This CT scan is a follow-up of the previous patient which confirmed the presence of a crayon in the nose.
Nose – Removal
In order to safely remove an object from the nose we’ve got to see it and identify its shape and what it’s made of. All of these make a difference in how we get it out. We use head-lamps, nasal specula, x-rays and CT scans; sometimes even MRIs.
Unless its round or easily breakable, or beyond “grabbability” for some reason, we most frequently can directly remove things using our tiny (and long) little “grabby” tools and hooks.
Next commonly we see if we can “snake” a small balloon catheter through the nose past the object then inflate the balloon and pull it back. If things go right, when the balloon comes back so does the object.
There is also the “positive pressure technique.” If the child is old enough to blow their nose they probably have already tried doing it. Otherwise someone (usually a parent) can plug the opposite nostril from where the object is by pressing firmly, put their mouth over the child’s mouth making a seal and then blowing quickly and firmly.
The reason that works is: 1 – the child is usually breathing out when you do it which adds to the pressure; and, 2 – pressure coming in from the mouth is forced “around the corner” and back up into the child’s nose. Enough volume of air being expelled out the nose often expels the object or at least “bumps” it further out where it can be reached.
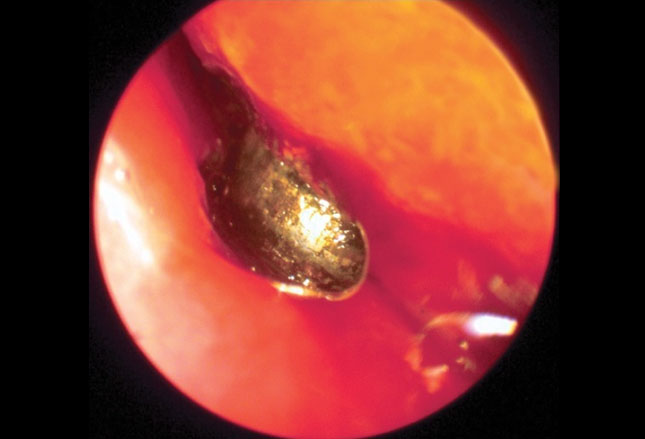
Objects with smooth surfaces which are easily visualized, can sometimes be removed with suction or glue on a probe. The image shows an intraoperative endoscopic view of a button battery in the right nasal cavity.
Eyes
My medical book describes: “Ocular foreign bodies may be protean in presentation, outcome and prognosis”—YA THINK?!
The picture I was going to show you is just too “grody” to even think about – a bungee cord hook in the eye – so I’m not going to show it.
Most common objects in the eye have been thrust there from using a hammer or power tools; and, the final resting place of, as well as the damage caused by, an ocular foreign body is dependent on its size, shape, and momentum at the time of impact in addition to the site of penetration.
We’ll talk about superficial corneal foreign objects in a minute but intraocular foreign bodies penetrate the anterior chamber of the eye or the globe itself and require rapid transport to an emergency room.
X-rays and CT scans help identify the extent of the injury. Sedation is often given to help control involuntary eye movement and surgery is frequently necessary.
Cornea
Most people know about “foreign things” in their eye because they have had some. It scratches, feels huge, makes your eyes water and is terribly uncomfortable.
We also know that most of the time the people you BEG to help you remove it say: “I can’t see nuthin'” and you end up trying to wash it out or using the “pull the upper eyelid down over the lower and let go” trick. Most of the time this works, even when you can’t see anything.
If the sensation doesn’t go away or you can see something in the cornea it’s best to see urgent care or emergency room to have someone with a practiced hand and special tools remove it—needlessly ruining someone’s eyesight trying to extract it is a high price to pay. If objects are not removed in a timely manner, infection or ocular necrosis may develop.
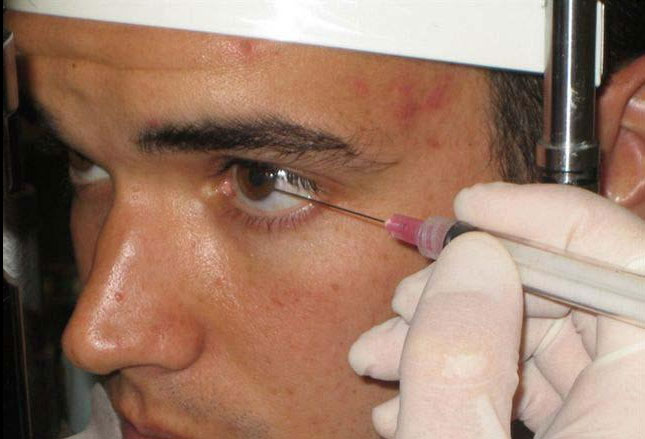
The photo shows a removal of a metal fragment in the emergency room; but, just as important is the exam with the microscope to make sure there is no penetration, the subsequent dye test to make sure there is no other damage to the cornea, any eye medication that is needed and any preventive bandaging required.
If there is ANY penetration, the child needs to be seen by an opthamologist (see section above).
Vagina
For boys, the nose is the clear favorite hiding place for “things.” For little girls however, the vagina runs a close second in the number of foreign bodies removed in the ED.
Depending on the object, physicians consider abuse; but, even in older patients things like tampons are not that uncommon. Some items if not removed promptly are prone to toxic shock syndrome.
Irritation, vaginal discharge, bleeding and a foul-smelling odor are all symptoms of retained vaginal objects which result from the inflammation and infection they produce.
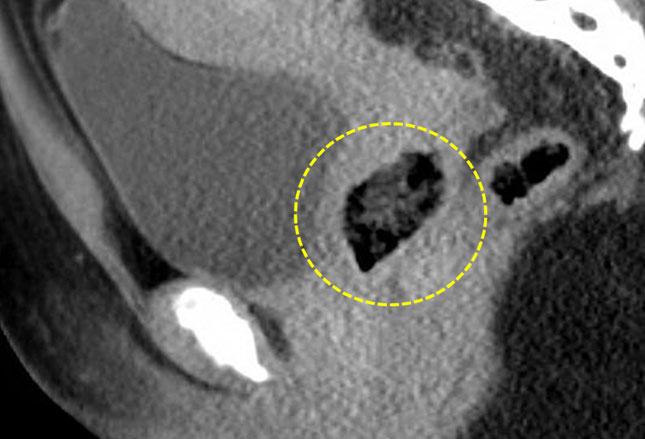
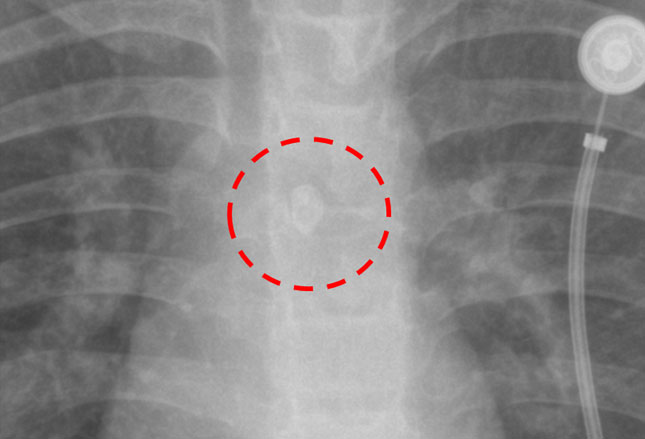
Removal of the object nearly always resolves the patients symptoms without other additional measures. The CT scan shows a vaginal foreign object (circled).
Bronchus and Lungs
Perhaps a mistake, but it looks like I’ve saved the perhaps most dangerous foreign body till last: the airways. They’re dangerous for reasons obvious to everyone who breaths for a living.
Young children, the elderly, those with neurologic disorders and decreased gag reflexes and patients undergoing sedation all are at particular risk; but, the Heimlich maneuver wasn’t invented because there was no need.
Stuff usually goes down the right main bronchus and into the lower pulmonary lobe, merely because of the way the lung passages normally develop. And the most common offenders are: (children) peanuts and other organic matter; (adults) vegetables, meat and bones.
There is usually a sudden onset of choking, shortness of breath, wheezing and coughing which, for older children, leads quickly to a diagnosis; for younger children, however, things sometimes are a mysterious investigation.
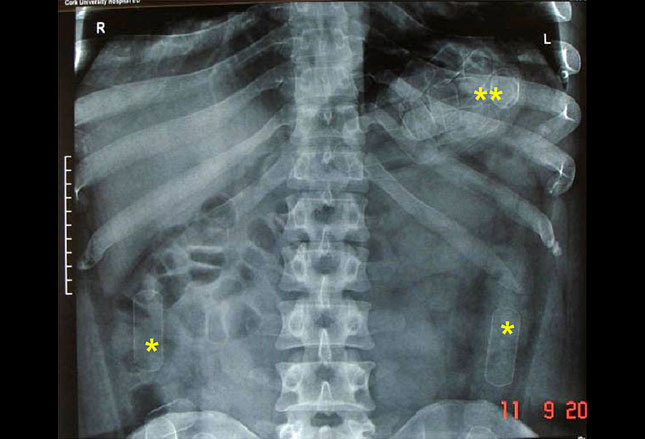
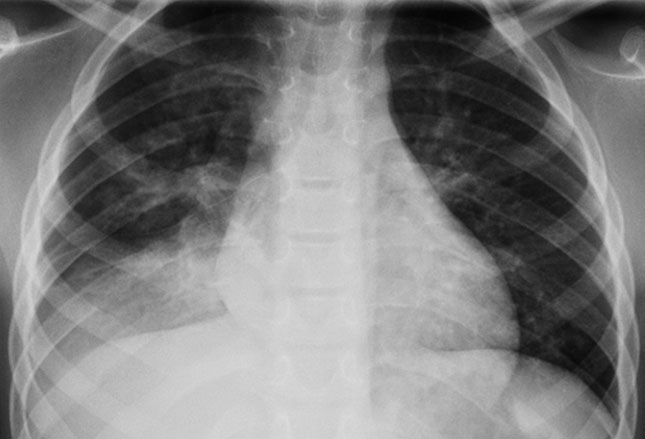
I’ve shown you already that chest x-rays can be used to identify radiopaque objects such as this tooth in the left mainstem bronchus (shown); but, not everything shows up on film.
Pneumonia
This is an image of what happens if an object isn’t readily recognized or treated timely—pneumonia and/or airway collapse.
Anyone with signs/symptoms of airway compromise should receive immediate chest compressions, back blows, abdominal thrusts or Heimlich maneuver, depending on the age of the patient.
Ultimately, whatever has been aspirated must be removed, hopefully by bronchoscopy but surgical extraction could be required. Unstable patients require expert airway management to avoid a poor outcome. Those who can still breath a little around the obstruction have a better prognosis.
Definitive airway management may be required in unstable patients. Overall, the prognosis is very poor for those with obstructive foreign bodies but excellent for those with nonocclusive foreign bodies.
Advertisement by Google
(sorry, only few pages have ads)