Physical Signs of Hidden Heart Disease in Children and Teens
Once upon a time doctors were almost thought of as wizards; not so much any more and it all has to do with the ability (and desire) to do a thorough physical exam.
No kiddin’. Before the invention of so much gadgetry physicians relied on their acute senses for ever-so subtle clues the body gives when it’s not running full on all cylinders but before a part gives out entirely.
An accurate diagnosis always begins with a good physical exam
Unfortunately, not only have many doctors begun thinking they’re too busy (or something) to do a good physical, some medical schools just don’t teach them how. And, double unfortunately, most of the time they get away with their complacency by pencil-whipping laboratory and imaging tests onto your bills.
The heart is a great example for what I’m saying. There used to be no greater “wizard” than an accomplished cardiologist in the days when all we had was our stethoscopes and an EKG (that’s what we called ’em before their name was changed to ECG).
Physical Findings of Hidden Heart Disease
So, let me give you some examples of what I mean. A lot of the subtle findings are literally too subtle to try and explain in writing and really need to be shown or demonstrated (which is why a physician goes through internship and residency training.)
Further, they are often too subtle to even photograph and/or would require a video. However, I believe that I can still come up with enough of the more obvious and easier to demonstrate/photograph physical findings that I can make my point; although, it hasn’t been easy to find photos.
Livedo Reticularis

I’ll begin with an example from my own training experience with Dr. George Veasy, cardiologist extraordinaire at the Primary Children’s Hospital in Salt Lake City—where I trained.
Our first day on the rotation was in cardiac clinic and our first patient was a completely new referral from a pediatrician in Ogden Utah. A teen was sitting on the exam table in his shorts and we could all see an unusual and worrisome rash on his ankle and foot.
The first question Dr. Veasy asked after introducing himself and us (and before even touching the patient) was: “has he had his cholesterol checked recently?” You see, when it’s presented like this it’s not really a subtle finding but it’s about as much a “back-door” diagnosis as it ever gets!
That day we learned about “Livedo Reticularis” (a rash due to diminished blood flow) and cholesterol embolisms. In hereditary hypercholesterolemia, which as it turned out this boy had, there are reasons that a cholesterol plaque can break away and cause an embolism.
About 34% of patients have skin findings as a sign they have such embolism. Livedo reticularis is a mottled, erythematous discoloration which blanches on pressure and may be associated with an actual area of cyanosis.
The rash is also associated with a whole lot of other diseases, some quite significant and others less so; but, my point is that an astute physician who takes the time to look thoroughly can save both himself and the patient a lot of time “barking up the wrong tree” so to speak.
In this boy’s case, a few simple lab tests diagnosed a family with fairly significant cholesterol problems, which could then be treated. It would have been too bad to have neglected to have him remove his shoes and socks merely to save time.
Erythema nodosum

Within a week of seeing the above patient Dr. Veasy was asked to do a consult on a patient who had been admitted through the ER with a leg rash which had been treated with two courses of antibiotics but didn’t heal.
He let two of us students go look at him first to see if we could come up with something; and, we actually did a creditable job—except, I must confess, we had a bit of help from the fact that I had worked one whole summer in a lab.
The advantage was that the rash had already been biopsied and my standing right next to the pathologist looking at the slide revealed Erythema nodosum, a rash seen in 25% of patients with Sarcoidosis—an idiopathic (unknown cause) inflammatory disease which effects multiple body systems and has many different presentations—and therefore is hard to diagnose.
Sarcoidosis mainly involves the lungs but 30% of the time also affects the heart. And when it does it’s usually with complete heart block—at a younger age than when from other causes.
The tissue biopsy was already done but we were then able to make sure his problem hadn’t yet affected his heart—which it hadn’t—although he did have the characteristic lymph nodes in his chest. Nor did he have renal involvement, which is the other organ system commonly involved.
A very early diagnosis made by an astute pediatrician enabling unusually early treatment for a complicated disease.
Erythema Marginatum

I have to tell you that there’s not much more difficult in the practice of medicine than accurately recognizing a rash which you’ve merely read about in books and seen pictures of. There’s absolutely nothing more educationally accurate than to actually see a person with the disease and his rash in context and to be able to see and feel it from many angles in multiple kinds of lighting.
Such is the case with Erythema Marginatum, the rash of a child’s first attack of acute rheumatic fever (ARF); which, as rashes go, is one of the more interesting rashes to see.
I was able to see 3 or 4 during my training; but, because ARF has been largely eradicated in the US, I haven’t seen it in the last 30 or so years… knock on wood! I don’t know how the young docs are learning it these days except in books.
As you can see, from the unusually clear photo and rash, it is a bit lacy, winding, pinkish and very slightly raised above the surrounding skin—usually with clear margins. It doesn’t itch, is mostly on the trunk and proximal extremities and resolves fairly quickly—occurring in only 10% of children with their first attack and 5% of children overall.
ARF occurs in children who have had recurrent “strep throats” that either haven’t been recognized and treated or who have not been treated with the correct dose for the full length of time necessary. On one of the subsequent infections (could be months or years later) the body begins to react with inflammation directed against some other organ—most frequently the heart. (Others are the kidneys and the joints)
Because the carditis effects the pericardium, epicardium, myocardium, and endocardium, ARF is considered a pancarditis.
There are two things which lead a physician to miss the early diagnosis in a child whose body is going to the trouble of warning them by sprouting the little-seen rash: not KNOWING about it, or not BOTHERING to look for it. It would be a shame to entirely miss an early diagnosis because it took too long to remove clothes to do an exam.
Acanthosis Nigricans

This next one, unfortunately, isn’t getting less… it’s getting worse and more frequent. Acanthosis Nigricans is a darkened, bumpy rash that changes the texture of the skin somewhat and makes it prone to grow skin tags.
If YOU saw this rash on a patient you would be pressed to do a certain kind of laboratory test—can you guess which one? A simple fasting blood glucose level, for diabetes.
This rash can be caused by a few other issues but is so well associated with insulin resistance that unless the patient already knew he/she was diabetic you ought to screen them for it.
Take a second look at the rash. Would you notice it if you weren’t looking for it? How about it, do you think you would see it if you decided you were too busy to ask the patient to take off their shirt?
The newly-coined term “metabolic syndrome” is, perhaps single-handedly, ruining the health of the country (and I supposed the rest of the developed world too). While cancer, AIDS and even things like SIDS are being corralled and controlled, obesity (and its associated metabolic syndrome) are exploding. Who’s responsible for solving this? Doctors have no “pill” or “treatment” to cure it.
Plus, the metabolic syndrome is not only a risk factor for coronary heart disease it leads to diabetes, fatty liver and several cancers as well.
Strawberry Tongue
I know it’s unusual that I say this; but, I hold a peculiar fondness for Kawasaki Disease. Yea, I admit its odd but it’s all due to a patient that came into clinic, let me diagnose it for him and let me care for him the several years I worked at that hospital.

The youngster was just so endearing, gentle and gracious that I can still not only clearly see his face looking up at me when I close my eyes; but even distinctly hear his voice in my memory if I think about him. To borrow the phrase from the book “the Little Prince,” the boy just totally and completely “tamed me.”
He endeared himself to me and, for better or worse, his disease seems to have tagged along: Kawasaki disease, it was a hot topic in my residency. It had been written about extensively in Japan, where it was first noticed and was apparently rampant; but, it had just begun to be seen in the US.
When I entered the room and made my usual silly introduction of myself to a new patient in an attempt of endearment; he just seemed to look up at me with a no-nonsense look like an old bank president, then matter-of-factly stuck out his tongue and said: “look what I’ve got.”
I stopped my silliness, smiled and said “Wow… now that’s something… how did you do that?” While inwardly thinking: “Oh crap!!”
Something told me that it wasn’t the strawberry tongue that might be seen with a strep throat, and I was right. I examined him from head to toe, drew some blood work and had them wait for the results, then admitted him to the hospital.
It was our hospital’s first case of Kawasaki’s disease, an acute, febrile, vasculitic, syndrome, of early childhood which started with red lips, strawberry tongue, peculiar rash and often ended with hospitalization due to some crappy side-effects.
The rash is due to the fact that the blood vessels are inflamed. The tongue and lips are red because the vessels are inflamed and the side-effects are because the vessels are inflamed—the heart and kidneys.
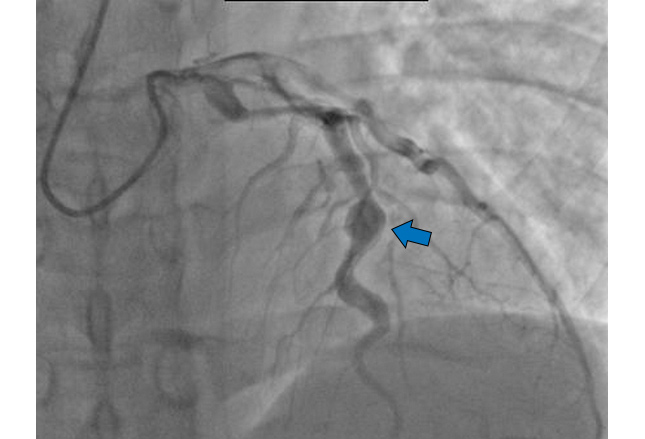
The most serious complication is a weakening of a damaged artery in the heart which causes an aneurysm; which can, and had, led to death—a Coronary artery aneurysm.
More than once I was grateful for the Japanese who had studied and written about the disease for several years. So many little-ones had gone before over there and even died that some treatments had been developed and I was able to use them on my patient.
A lot of things give a child fever, even high and prolonged ones. A lot of things give children rashes, not so much on the hands and feet. Many things cause “pink eye” or red tongue or red lips or swollen lymph nodes.
But, unless you do a good job at a physical exam looking at everything many of those things won’t be seen much less the swelling and/or peeling of the hands and feet, tiny splinter hemorrhages or swelling around the anus.
These days they’ve developed a list of criteria which, when met, indicate Kawasaki Disease because we have no lab test for it. However, especially for the large percentage of children who develop cardiac involvement just at the time they are beginning to heal, making the diagnosis is critical because treating early can prevent the BAD things from even happening at all!

Prompt treatment with intravenous immunoglobulin (IVIG) and high-dose aspirin is the current standard of care. Coronary aneurysms (shown) occur in 25% of patients not treated with IVIG, compared with approximately 1-5% of patients treated with it.
Aspirin has a synergistic effect with IVIG, so it is initiated at a high dose. Aspirin may be continued at a lower dose for its anti-platelet effects to further reduce the risk of thrombus formation.
If a doctor misses the diagnosis until the child begins healing, i.e. the fever is subsiding, then they’ve missed the best chance to help because that’s when the risk of sudden death is the highest from a coronary aneurysm.
Janeway Lesions and Osler Nodes

A lot of diseases are difficult to treat for a physician but there is absolutely NOTHING fun about Janeway lesions or Osler Nodes; that’s because having a patient who has an infection growing INSIDE him, especially Staph Aureus, just scares the begeebers out of a doctor who is in his right mind.
A teen who develops fever and chills, a new heart murmur (of just about any type) and has a big toe that looks like this (shown) has just about always developed acute infective endocarditis, inflammation of the lining of the heart. And, it’s nearly always caused by Staph Aureus; because, those are Janeway lesions on his toe (or finger, or palm or sole).

Take the same patient but with a little longer onset and a rash like that on his hand (shown) and it’s most likely subacute bacterial endocarditis from Strep viridans; because those are Osler nodes. Osler nodes are painful, red and most common on the pulp of fingers and toes.
These photos are the most obvious examples I could find for you to see; but, believe me, they are nearly always much, much less obvious and in many cases are missed entirely by the first doc who sees the patient, unless he/she does a thorough physical exam with his eyes wide open and his mind full of suspicions.
Splinter/subungual Hemorrhages

Not to be left out, there is another common (but often subtle) finding in infective endocarditis: subungual hemorrhages, often called “splinter” hemorrhages.
The mortality (death) rate of acute endocarditis is as high as 50%; so, it tolerates no delay in diagnosis and treatment.
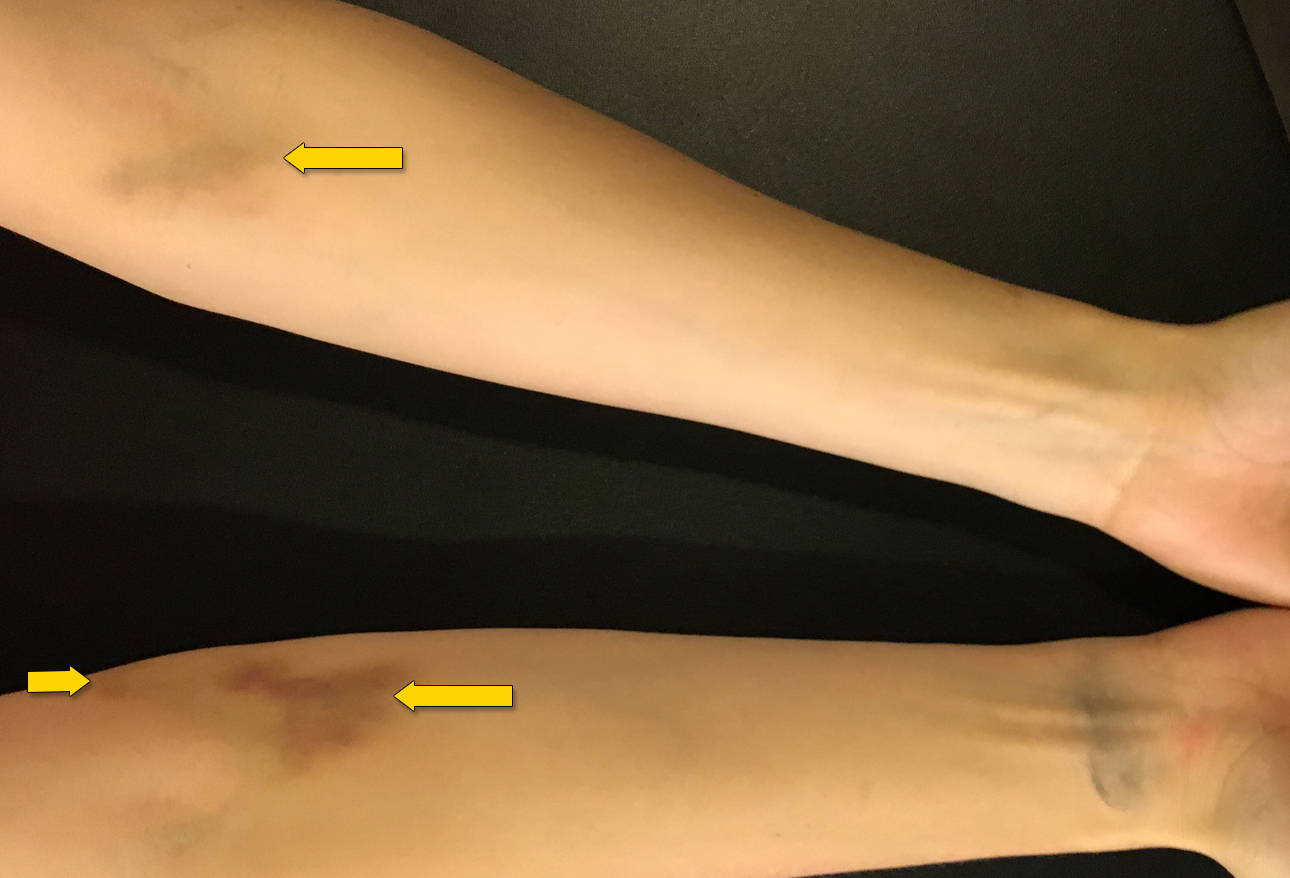
Drug use directly into the vein (IV) is a common cause of infective endocarditis, even for patients without any other symptoms whatsoever. Almost 86% of IV drug users have a skin manifestation or complication due to drug injection.
“Users” inject into the cubital fossa, arms, fingers, toes, legs and neck which cause bruising, puncture marks and scars, cellulitis, abscesses, inflamed veins and scarring.
☤
There is absolutely nothing more comforting than stumbling upon or finding a physician who takes the time to do a good physical exam; and you should feel lucky.
Advertisement by Google
(sorry, only few pages have ads)

