Puberty, Acne and Beyond – Most Internet Information Wrong
It’s called Acne Vulgaris, and for most children in the throws of the crisis called Puberty the name pretty much sums up how they feel about it. It is the most common skin disease of any and pretty much hits 80% of us at some time or another.
The issue is that our skin has “pilosebaceous units” all over it, made up of a hair follicle, its accompanying sweat and oil glands and the erector muscle which connects to it. Each of these have their own issues trying to grow and do their jobs; which, especially in puberty, seem to all lead to pimples.
Moderate acne on the face of a teen boy
That means acne is “multifactorial” – with many causes; like: androgen-induced sebum production, hyperkeratotic plugging, increased number of Propionibacterium acnes bacteria and inflammation which, once started, produces more of itself.
Acne Increases At Puberty
Acne can range from mild to severe and as such may reek havoc on the distress level of a newly-developing teen with symptoms such as: anxiety, depression, social withdrawal and even suicidal ideation.
Home remedies (even oddities found on the internet) often are tried first; but, it’s often critical to discover a proper diagnosis and differentiation of its various forms before correct therapy can be given.
Acne Means Pimples
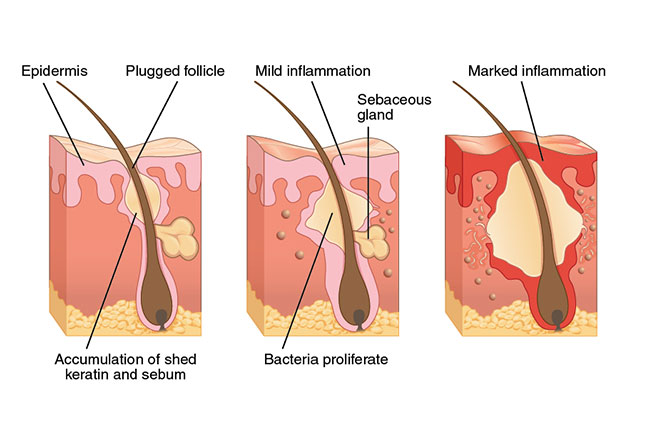
Doctors will tell you that “acne begins with the formation of the microcomedo at the infundibulum of the hair follicle.” In “normal” speak that means a very tiny plug forms right where the hair exits through the skin which therefore prevents anything else from exiting that route either – a microcomedo.
What else might want to exit that route? Well, dead skin cells for one (dead corneocytes) and oil for another. You see, there are oil glands that secrete right into the hair follicle to keep it flexible and working well. When there’s a plug nothing gets out and things begin backing up.
Androgens (the hormone class to which testosterone belongs) are like fertilizer and make everything grow – skin cells, hair, oil glands and sweat. Bacteria see all this extra growth and begin growing too (P acnes) which then triggers other body cells to flock to the area and “inflammation” begins.
Oil gets thicker, mixes with dead cells and begins compacting tighter and tighter forming concretions and a Comedone (pimple) is born. At this point we call the problem: non-inflammatory acne.
If the force builds up so much that the tube ruptures, however, all that dead skin, sebum and inflammation spill out into the surrounding skin triggering another reaction out there. That is how papules, pustules, nodules, and cysts are formed – which we call inflammatory acne.
Non-inflammatory Acne
To the right is a photo showing both the open (left) and closed (right) Comedones of non-inflammatory acne.
Open Comedones are known as “blackheads” and are basically the widened openings of hair channels which have been filled with keratin (the outer casing of dead cells). We guess that the melanin which gives skin its color and the oxidation of the skin oil as it sits and thickens is what gives blackheads their characteristic color.
Closed Comedones are what most people call “whiteheads” or just “pimples.” They are basically skin-colored and not erythematous (reddened) and they don’t have an opening through the skin as a normal hair follicle would have. They seem to show up better on photographs because of the side lighting.
The first treatment for both types is to try and cleanse the skin of dead cells which might open the pores. This is done with medications known as retinoid, azelaic acid and salicylic acid, all of which tend to increase dryness, flaking and a slight reddening; although such effects do diminish with continued use.
Sunscreen is also important for all persons who use topical treatment like this because they make you more susceptible to sunburn.
Inflammatory Acne
As stated above, when the pressure of all the material gathering inside a comedone ruptures out into the surrounding skin it produces redness and inflammation – inflammatory acne.
The bacteria grow and expand to take on several different appearances: papules, pustules, nodules, and cysts. Papules are generally 1-5 mm in diameter. The photo shows a moderate case of inflammatory acne in a teen boy with many erythematous papules and some closed Comedones.
To treat acne at this stage requires the use of an additional topical antimicrobial agent in addition to the retinoid therapy. We use benzoyl peroxide, clindamycin and erythromycin because we know that the two products work better when used in combination.
Pustular Acne
From here on out we’ve got different names for acne as the inflammation is deeper and more pronounced. The photos become more and more difficult to view as the disease becomes more disfiguring.
Pustules are larger and deeper into the skin than papules and are filled with yellow fluid which contains cellular debris and bacteria as well as a lot of the bodies of inflammatory cells which are trying to kill all the foreign matter. And they are much more painful to the touch.
Treatment now includes not only topical retinoids and antimicrobials but oral antibiotics as well which will penetrate the deep tissues more effectively. Tetracyclines are typically used in teens.
Cystic Acne
Here is where nearly all of the rhetoric found on the internet begins to be completely wrong. 1- Don’t believe the photos, they’re mislabeled; 2- claiming any type of “oil” will help is stupid and inappropriate; 3- claims are falsified and exaggerated; and 4- absolutely nothing sold on the internet to “cure” cystic acne has no basis in fact – period!
Why is this a big deal? Because if a child has true cystic acne then the longer it is untreated the deeper it digs and the more entrenched it becomes. It can go from a significant acne issue to a recalcitrant malady that is so difficult to treat it might take years and leave needless scars.
The very LAST thing a child needs to be doing is following some mercenary con-artist trying to make money off their desperateness and delaying both diagnosis and treatment.
Photos of true cystic acne are painful to view so this photo is of a mild example and, fortunately, will probably be successfully treated fairly rapidly – but by “rapidly” I don’t mean before the prom next month AND absolutely NOT BY ANYTHING AVAILABLE FOR PURCHASE ON THE INTERNET!
The acne process is the same but the inflammation has now not only spread into the surrounding skin but has also begun causing cysts, a pus-filled pocket under the skin which is painful to touch.
Perhaps this girl has “pseudocysts“, it’s difficult to tell without being actually able to examine them closely and touch them. Which is why absolutely ANY ADVICE for treatment of cystic acne which DOESN’T begin with “see a dermatologist” is dangerous for your health and must not be given credibility.
Even us pediatricians might begin treatment for cystic acne but will refer to a dermatologist for additional treatment and advice; BECAUSE, the treatment most often includes injection with medicines which, if not done with skill, can actually lead to more scarring than the acne alone!
Nodulocystic Acne
Now, if you won’t mind, let me skip the photos for the next few classifications. They really have no useful purpose outside of a medical teaching setting; but, I will give a description which should be easily extrapolated from the photos I’ve shown already.
Nodulocystic acne is basically deeper in the skin and has both cysts and nodules in addition to the more superficial comedones, papules and pustules. The medication isotretinoin is used as first-line treatment, taken orally for 4-6 months and is not without it’s own side-effects: cheilitis, xerophthalmia, epistaxis (secondary to dry nasal mucosa), and eczema.
The most adverse side effect is fetal teratogenicity which is why it’s only available from a doctor’s prescription in carefully diagnosed conditions and with many precautions. A newer version of the med has been approved (CIP-isotretinoin) having better absorption but, sadly, the same side-effects.
Acne Conglobata
Acne conglobata is both severe and rare and is usually seen in combination with other problems such as dissecting cellulitis, hidradenitis suppurative and pilonidal cysts.
It tends toward young males and is located on the chest, back and buttocks forming extensive cysts with sinus tracts and communicating abscesses with purulent drainage. Treatment obviously includes antibiotics but nearly always needs other medications as well, and surgical intervention.
Acne Fulminans (acne maligna)
The most severe form of acne, Acne fulminans or maligna, mainly affects white male teens between 13 and 16 and is thankfully very rare. It is sudden (after a year of “normal” acne), forms ulcerative, pus-exuding lesions and is associated with other bodily symptoms like fever, arthritis, muscle aches, malaise and liver and spleen enlargement.
It changes laboratory findings and involves bones so most patients end up with radiographs and perhaps bone biopsies. Treatment is very tailored to each patient with many of the above procedures plus oral steroids. The problem may also herald that the patient has/is developing other syndromes.
External Causes Of Acne
Drug-related acne
Several drugs, including steroids, will cause an acneiform eruption. Drug induced acne is usually asymptomatic, red, monomorphic papulopustular rash with no comedones. In other words, all the lesions look alike as if the same age.
Some cancer drugs and exposure to chlorine are two other causes. Drug related acne breaks out in more unusual locations than is seen in other types of acne, and it can be resistant to conventional acne therapies.
Steroid-induced Acne
Normal puberty related hormones trigger the onset of acne over time, receiving hormones artificially will trigger acne as well – like those receiving treatment for allergies and those illicitly trying to bulk-up for sport’s reasons.
Some drugs characteristically produce lesions around the mouth, others on the chest and upper arms.
Steroid Abuse Acne
The thing about “doping” acne is that it can be any of the above types right up to and including the dangerous Acne Fulminans and it occurs in at least 50% of “dopers.” And, if athlete’s are doping with steroids they are nearly always using vitamins as well – some of which also cause acne.
Other signs of abuse of these agents include gynecomastia, decreased testicular volume, striae, edema, and increased body mass index.
Acne Mechanica
The friction of repeated mechanical obstruction can plug up the sebaceous glands and form comedones of a type known as Acne Mechanica. Chin straps, collars, suspenders, helmets, crutches and the like are all culprits.
Some causes have even been given their own special name like: Fiddler’s neck or Violin hickey. Diagnosis is usually made by the well-demarcated geometry of lesions.
Neonatal Acne
About 20% of newborns develop “neonatal cephalic pustulosis” on their cheeks and nose within a couple weeks of birth which lasts up to 3 or so months. Most people just call it: Neonatal Acne.
Most likely it’s due to stimulation of the sebaceous glands from maternal androgens; but, it is self-limiting and benign. In particularly persistent cases topical imidazole agents are sometimes used.
Infantile Acne
It should be said that infants three to 12 months (mostly males) can also develop classic acne with comedones as well.
It can be treated with similar drugs as used in adolescent acne although erythromycin is the preferred antibiotic due to significant side-effects from those used in older children.
Occurrence this young can sometimes be a harbinger of adolescent acne incidence and severity.
Postadolescent Acne
Lastly, acne can still persist (or even begin) after adolescence has ended. More women older than 25 years are affected and it seems to relate to menstrual cycling.
Lesions are often painful papulonodules along the jawline and neck and unfortunately may be resistant to multiple courses of antibiotics. Treatment is aimed at controlling androgen levels with varying medications but care must be taken in women of child-bearing age because they can feminize a male fetus.
Complications Of Acne
Acne which is more than just a few open or closed comedones runs the risk of developing several types of physical complications – that is, those above and beyond that of the emotional and psychological issues there might be.
It’s related to how much disruption of the dermal layer (the actively reproducing deep skin layer) there is. Inflammation which breaks out of the comedone into the surrounding tissue, as many of the above mentioned types do, may cause changes in the above skin sometimes long after the original acne has resolved.
Postinflammatory hyperpigmentation
A not particularly uncommon complication of significant cases of acne is hyperpigmentation – darkening of the skin pigments.
The process of inflammation caused by the acne can darken the skin color in localized areas and is most often only temporary but can become permanent independent of whether or not there has been scratching or popping etc.; most frequently in dark-skinned individuals and those with certain genetic skin types.
We do have some medications that can help (prescription hydroquinone) much better than over-the-counter meds; and it can be mixed with other enhancing meds by a doctor, tailoring it to individual needs. Best used as “spot treatment” but also as “field therapy” on more diffuse cases. There is a potential of a ring of “hypopigmentation” around each lesion so care must be taken.
Scaring
If the inflammation is severe enough, it can lead to scaring of three different types: Ice-pick, boxcar and rolling. Adequate treatment is key to preventing progression into any of the types which can occur either singly or mixed.
Ice-pick scars, by definition are sharply demarcated, narrow and extending deep into the dermis or subcutaneous tissue. The depth is greater than conventional treatment by resurfacing can reach so usually undergo punch excision or grafting.
Rolling scars have a rolling, shallow appearance due to their unusual fibrous anchoring of the dermis to the subcutaneous tissue.
Boxcar scars are round to oval with sharp vertical edges either shallow or deep.
Treatment needs to be completely individualized but is usually surgical. Even the latter two types can be treated with dermal filling, resurfacing, or surgical subcision (subcutaneous incision).
Acne excoriée des jeunes filles (“excoriated acne of young girls”)
Remember when your mom told you that if you picked at your scabs you would get a scar? You don’t? Well, maybe it was a ‘guy thing.’ Well, even though you might not have seen it happen on your scabs, it turns out that she was right.
Comedones and inflammatory papules that patients have habitually picked and scratched will not infrequently scar and it’s common enough in acne that it’s been given its own name: Acne excoriée des jeunes filles – or translated “excoriated acne of young girls” because that’s where it is seen most. And more often in those with a history of obsessive-compulsive disorder, depression, or anxiety.
Treatment of this fairly rare condition often requires psychiatric intervention and medications similar to those used for tics and other skin-picking compulsions can be useful (except, that a side-effect of some of them, i.e. lithium, can be acne).
Solid facial edema (lymphedematous rosacea, Morbihan disease)
A more rare complication of acne is the “firming” of the sub-surface edema into lymphedematous rosacea (Morbihan disease). It is usually on the mid-face and is what we call “non-pitting” on examination.
Perhaps it is due to impaired lymphatic drainage, we don’t really know, but it occurs in late teens and early 20-year-olds who’ve had a long history of acne. It can persist indefinitely if left untreated, and it may lead to visual impairment if left uncontrolled.
Being rare it might not be diagnosed early unless the doctor is aware and looking for the condition and is one where family practice and pediatricians should seek consultation with a dermatologist who has experience with its treatment.
If resistance is shown to the medications used, plastic surgeons may need to intervene for debulking or eyelid complications.
Diagnosis and Treatment Of Acne
Diagnosis Of Acne
You think that this is just a common malady and shouldn’t be more difficult than changing a tire – and for the most part you are right. However, for perhaps 20-30% of kids with the problem it’s more than just a passing inconvenience and they need more than OTC (over the counter) medications and tincture of time.
If acne becomes more than 2 or 5 pimples at a time, or they tend to linger and turn red; then, they need “proper” treatment and for that you owe it to them to have an accurate diagnosis in the first place where some of the “bad” causes can be “ruled out.”
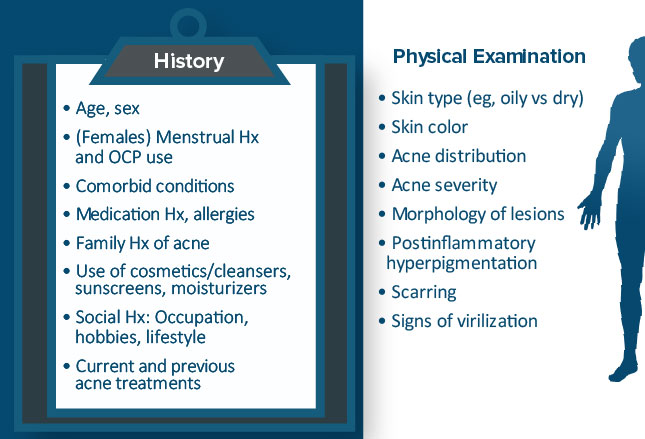
After a relevant history and head-to-toe physical it will be great to know that they have none of the real problematic issues that will take correcting and/or make treatment substantially more difficult. The full physical can point to hormonal problems in both boys and girls without needing blood assays.
In girls it’s important to rule out the many causes of androgenic overactivity which make the acne merely a sign of a deeper problem and needs treating – the pimples are the same either way, it’s the rest of the physical that matters and it’s important to relate symptoms to menstrual cycles.
Androgenic activity is already present in boys but they can have overactivity as well – it’s just a bit more complicated to decipher. Click to expand the chart on the left to see history and physical parameters and notice that the abbreviation “Hx” stands for “history.”
Acne Treatment Options
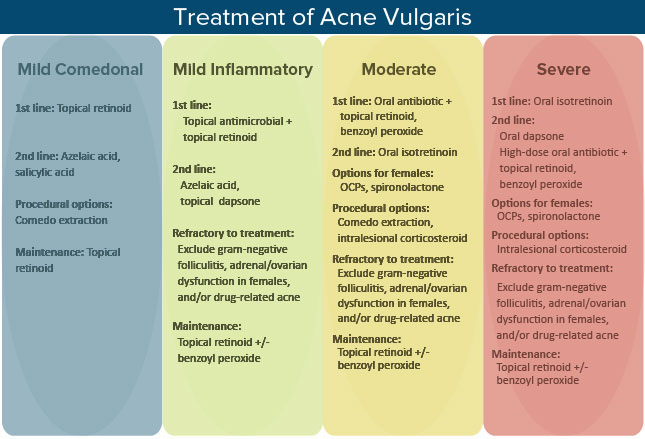
Like I’ve done above, the chart on the right is a summary of the various treatment options which we have categorized by the severity of the disease.
Topical retinoids (tretinoin, adapalene, and tazarotene) which normalize follicular keratinization and keratinocyte cohesion to treat existing comedones and prevent new ones.
Azelaic acid also alters follicular keratinization as well as inhibiting the bacteria P acnes’ proliferation making it especially effective against inflammatory lesions.
Salicylic acid is both comedolytic and anti-inflammatory but sometimes causes additional skin irritation.
Topical antimicrobials include benzoyl peroxide and antibiotics such as clindamycin and erythromycin.
In general, comedo extraction should be performed on the noninflammatory type lesions to prevent scarring, the other types need proper medical treatment and physical manipulation might actually make the inflammation more wide spread or severe. For intralesional corticosteroid injections the doctor will probably use triamcinolone.
Advertisement by Google
(sorry, only few pages have ads)