Children’s Bacterial Skin Infections
It’s incredible how popular the posts that I do with a “guess the answer” format have been. I usually try to make them about topics which train young parents in diagnostic or treatment skills that will help them keep their children healthy and safe.
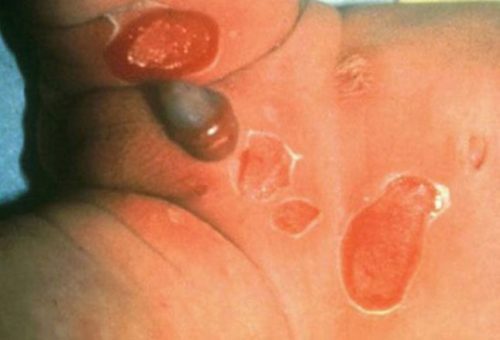
Diaper area rash of Staphylococcal Scalded Skin Syndrome
Today is no different. Skin infections in children are, perhaps next to ear infections and colds, one of the most common maladies we see. It is almost impossible to raise a child without going through at least one before they leave home.
Children’s Bacterial Skin Infections
Diagnosis, Treatment and Questions
We’ve talked about this topic before so today I thought I’d throw in a few not-so-common infections to not only make it interesting but give you an understanding what is going through OUR minds as we examine your child — and why we’re relieved when we don’t find them!
Peeling of Skin

You are seeing this 18 month boy who had a diaper rash in the last week then developed this rash over his body on the weekend. He has been very irritable.
To your practiced eye he just “looks sick” and does have a fever. The real problem is the desquamation (sloughing) of skin at the granular layer which leaves a wet-appearing surface beneath.
What is the best diagnosis?
A: Impetigo; B: Candidiasis; C: Staphylococcal scalded skin syndrome; or, D: Erysipelas
Staphylococcal scalded skin syndrome
The photo shows SSSS, as it is known, definitely NOT a good disease to have. It’s caused by the fairly common bacteria Staphylococcus but in this case the bacteria secretes a toxin which causes the surrounding skin to peel off leaving only the raw, weeping under-layer exposed – just like a burn or scalding, hence the name.
The site of skin sloughing often involves the face and neck including behind the ears even though the original infection with staph might be a distance away. Initially there is usually a central red rash which feels like sandpaper.
Children are prone to the syndrome because of lack of immunity and immature renal clearance ability to get rid of the toxin. Adults with chronic illness or renal failure can also get the syndrome.
Treatment of SSSS includes antibiotics (so far) and substantial fluid rehydration due to large losses through all the weeping skin.
“Bee sting gone bad”

A 16 year old boy comes to your office with what he is calling a “bee sting gone bad” on his shoulder.
He was working in the yard over the weekend but didn’t notice anything until he was getting ready for bed and saw a red bump like a “bee sting” on his shoulder.
The next morning it was quite a bit larger, red and tender. This morning the redness has spread to his armpit and it hurts to raise his arm. He has a slight fever.
What is the best diagnosis?
A: Necrotizing fasciitis; B: Impetigo; C: Botryomycosis; or, D: Lymphangitis
Lymphangitis
Lymphangitis, sometimes called “blood poisoning,” is the progression of an infection (often Streptococcus pyogenes) along the lymph channels which are draining the infected area. In the case of the shoulder the lymph drainage goes into the axillary lymph nodes, so that is where the infection goes.
An infection with this organism can rapidly progress leading to significant complications and patients can appear quite “toxic” along with their fever. They may have a history of a recent cut or abrasion which obviously gets infected. The red streak leading away from the site is the giveaway.
Children will usually have a fever which may be quite high, chills and malaise. Some report a headache, loss of appetite and muscle aches along with the local symptoms.
Not Your Mamma’s “Athlete Foot”

An 18 year old appears in your office accompanied by his mother after spending several weeks trying to treat his athlete’s foot problem. They had visited an “after hours” doc-in-a-box where the “doc” had given them prescriptions for athlete’s foot but this just wasn’t getting better – it was getting worse.
There were some “family dynamics” issues you could tell so took his mother into the hallway with you while the boy sponged off the ointment he had on his feet. She gave you a little more history then you went back, alone, to speak with the boy.
After asking him a couple of questions you had a suspicion that it wasn’t athlete’s foot (after all treatment hadn’t worked) so took a skin scraping and sent it in for a biopsy.
You weren’t surprised by the lab results but the family was when you talked to them next.
What is the most likely diagnosis?
A: Impetigo; B: Ecthyma; C: Pitted keratolysis; or, D: Syphilis
Syphilis
You thought Syphilis was a thing of the past didn’t you? It’s not; but, don’t feel bad because many of the new crop of physicians think the same thing.
Syphilis, we were taught, is the great mimicker and can present as just about anything. Until drug abuse became so prevalent physicians used to ask sexual activity questions of patients as much as we do drug related questions now.
Skin lesions associated with syphilis include papulosquamous lesions on the trunk and coppery patches on the palms and soles with a peripheral adherent scale.
There are laboratory tests specifically diagnostic of syphilis and in many cases a pathologist can stain samples of skin and find the actual treponemal organisms in deep layers, which was the case in this patient.
Honey Colored Rash

You’re in a big-box store and chance upon one of your patients and his family shopping. They live on a fundamental farm and have a large family size for this day and age; but, have some of the most hard-working, energetic, inquisitive and happy children in all of your practice.
Unfortunately several of the children have rashes around their mouths that you recognize as a problem so you mention to the mother that you should see them in the office soon so you can make sure of the diagnosis and begin treatment.
When they come in, each child has a similar honey-colored, weeping rash with a red base but in different locations. A couple are around their mouths but the oldest, 14, has the rash on his arm and shoulder.
What is the best diagnosis?
A: Ecthyma; B: Staphylococcal scalded skin syndrome; C: Botryomycosis; or, D: Impetigo
Impetigo
This infection is one of the most commonly acquired skin infections in childhood and is highly contagious, through direct contact. It’s caused most often by the bacteria Streptococcus, although Staphylococcus might overgrow the whole rash once it gets started.
Because it is so common and the rash is so distinctive, diagnosis can usually be made on sight without the need for cultures. However, if the physician knows that there is an outbreak of methicillin-resistant organisms in the community (MRSA) or there is suspected poststreptococcal glomerulonephritis, both cultures and sensitivities of the organism should be taken.
Daycare Nodule

An infant in your practice developed a “pimple” on her thigh a few days ago which is getting steadily larger, redder and warm.
She attends daycare during the week; so, when upon examination you find a fluctuant nodule (lump) you must consider it to be the result of an infection with methicillin-resistant Staph Aureus (MRSA).
Staph is one of those bacteria which have developed resistance to antibiotics so what should you do now?
What should be your initial treatment of choice?
A: Drainage; B: Oral sulfa drugs; C: Oral doxycycline; D: Oral clindamycin; or E: IV vancomycin.
Drainage
There is absolutely no doubt that an infection with MRSA is serious. It’s one of the bacteria which have mutated and now are resistant to the antibiotics we have always used which makes it deadly in many circumstances.
However, antibiotics aren’t the only method the body has of fighting bacteria and clearing it from the skin. “Normal” cellular defenses are excellent at the job IF given the chance. In the case of abscesses under 5 centimeters (almost 2 inches), they have been shown to have similar outcomes when treated either with or without antibiotics IF they are adequately drained.
The treatment of choice is therefore drainage by the “old fashion” method of “lancing the boil.” If we do that, the body almost always rids itself of the infection.
Using antibiotics can cause risks of their own, including the Stevens-Johnson syndrome. And Tetracyclines are contraindicated in children due to their effects on bone growth, except in life-threatening conditions such as Rickettsioses.
Delay For “Homeopathic” reasons

A boy you’ve seen since infancy has come to see you with “pimples” all up and down his legs. His mom had him accompany her to an appointment with her “family doctor” two weeks prior when he noticed a crop of pimples on his lower thighs after gym class.
The doctor, an osteopath who practiced homeopathic medicine, had talked about “growing up” and “stress” and “sweating” and “new skin bacteria” and lots of research about “new natural remedies” and said that washing with his “antiseptic” soap three times a day and using his “stress reducing” treatment which has research showing it improves “over sweating” should easily resolve the issue.
It didn’t, in fact she said: “over two weeks it got worse and the doctor had called in Cephalosporin antibiotic for him to take; but, it wasn’t doing the job either – and thanks for working us in today, his gym teacher wouldn’t let him dress because it might spread {quick breath} and he just has to play in the game this weekend! And we really can’t afford to use that cream any more when it’s not working!”
There has been no hot tub use or wading in unchlorinated waters; but, he knows someone who has had the same rash – his basketball point-guard neighbor last month. Just looking at the rash, it’s obvious that he has folliculitis with areas that have coalesced into furuncles on both thighs.
So, what is the REAL treatment? A: Drainage of individual lesions; B: Oral sulfa drugs; C: Oral doxycycline; or, D: Oral clindamycin