Sudden Cardiac Death in Child Athletes
Sudden Cardiac Death is, by definition, both sudden and unexpected – especially in a child whose life is supposed to revolve around “play” and “fun.” Unfortunately, it is also increasing.
Just as unfortunate, children’s “play” is often “industrialized” into major competitions with adult methods, standards and expectations leading to unintended consequences.
Sudden cardiac death often, but not always, occurs in athletes
Sudden Cardiac Death
Figures for the “incidence” of sudden cardiac death in athletes vary all over the place (from one in 50-300 thousand); because, how can we possibly ever know the true “denominator” – i.e. know many total athletes there are.
We DO know however that in the US general population 2 in 1,000 people die every year from sudden cardiac death. Multiply that out and you get 300,000 people dying each year. Among the general population Males are disproportionately dying over females, nine to one; and blacks slightly more than whites.
A study of 2,149 US high schools between August 2009 and July 2011 (> 2 million students, > 750,000 athletes) found 26 incidences of sudden cardiac arrest (SCA). 18 were in athletes, 7 in non-athletes – all occurred during exercise.
The incidence of SCA in boy athletes is 1.73 per 100,000 – much more than the 1/100K that we had previously estimated. Comparing that with the girls and non-athlete’s incidence of 0.31/100k is not comforting at all!
Athletes And Their Hearts
If you look at a runners legs you can plainly see their well-defined muscular calves resulting from adaptation to the exercise. You’re not surprised that their heart muscles have also adapted too – are you? Both in males and females and in all sports?
You can spot the heart’s growth on x-rays, echo’s and ECGs. It enlarges, thickens and slows (bradycardia) and, here’s the rub, sometimes it alters in the way it “fires” – i.e. changes its electrical conduction through the heart and “throwing in” extra beats. Commonly these are premature ventricular contractions (PVCs), the stuff “heart attacks” are made of.
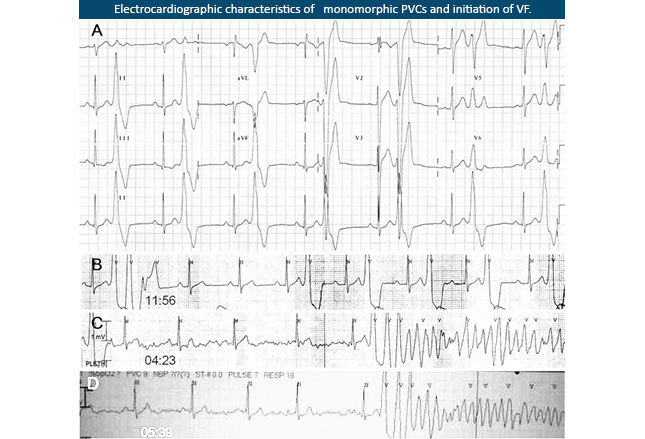
The example (left) is the ECG tracing of a 17-year-old boy who was resuscitated from a SCA and was monitored in the CCU.
There are four different rows showing how “mixed up” his heart’s firing had become. The bottom row shows him going back into another “attack,” ventricular fibrillation (VF), from which he needed to be electro-converted (shocked back into regular rhythm) again.
Causes Of Heart Changes
The whole purpose of the body’s response to exercise is to make it more capable of delivering the increased amount of work required. In the heart, ventricular walls thicken and the cavity dilates. Both of which change the organ’s functioning to increase pressure or volume pumped. And, what goes up with exercise can come down with de-conditioning.
These structural changes can be physiologic (responsive and “normal”) or pathologic (unusual and damaging) or both. Aerobic activities like running tend to increase the ventricular cavity’s dimension – to pump more volume. “Power” sports like weight-lifting usually increase the wall thickness – for more “push” (pressure) against tense vessels (squeezed by muscles).
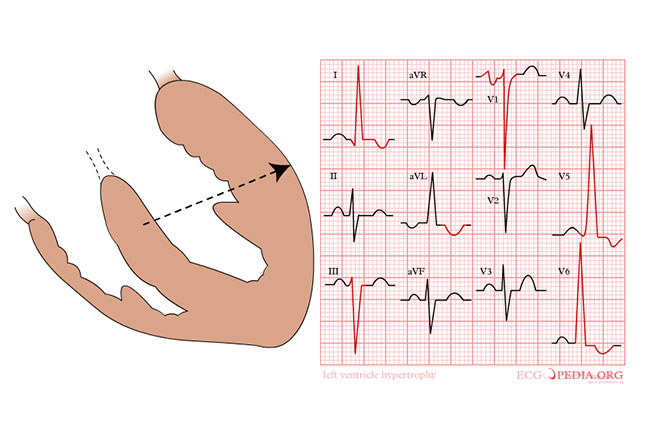
If the heart muscles enlarge asymmetrically it can harm effective output and trigger arrhythmias. An ECG might be able to pick that up but not always. Inheriting some genes can also contribute to cardiomyopathy.
Grinkov Risk Factor
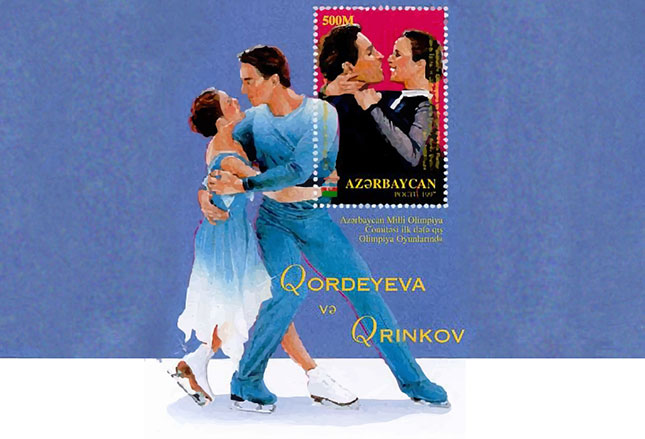
One of the genes we’ve discovered which causes cardiovascular abnormalities is now known as the Grinkov Risk Factor – mutation in the “PLA2” gene.
When inherited, that gene mutation causes advanced coronary artery disease like in Sergei Grinkov and his father, who both died early of the problem. Sergei was a Russian pair figure skater; who, with his wife, was a two-time Olympic champion.
In 1995, while in Lake Placid New York rehearsing for a tour, Sergi had a fatal myocardial infarction. That lead to the autopsy, the discovery of the condition and the gene that caused it.
Since then, other genes have been discovered which effect heart functioning – fortunately, they are quite rare.
Conditions Leading To SCD
There are several conditions which can produce sudden cardiac death; but, unfortunately, there are often few warning signs for many of them.
Most are uncommon but I’ll list a few of the “more commonly uncommon” so you’ll know what I’m talking about.
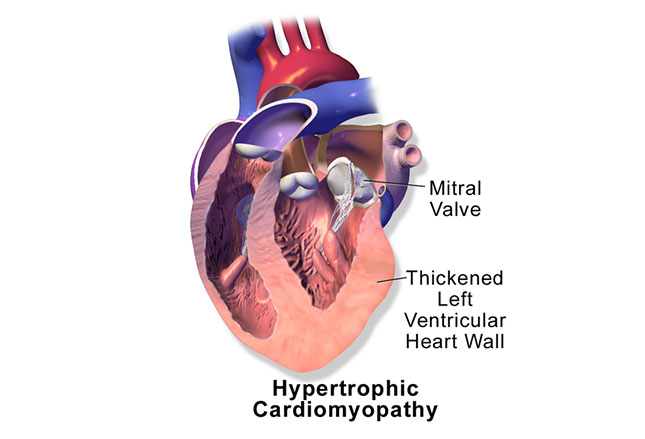
For athletes it includes hypertrophic cardiomyopathy (HCM), Commotio Cordis, coronary artery anomalies and coronary artery disease (CAD).
In the general population it’s mostly coronary artery disease but also valvular disease, HCM and mitral valve prolapse.
Hypertrophic Cardiomyopathy
Despite being relatively uncommon, Hypertrophic Cardiomyopathy often “makes the press” due to the tragedy of an unexpected death in a very young athlete. And it’s very difficult to get a handle on preventing it despite a lot of testing because there is no warning.
As I’ve described, enlarged heart muscle is what we find when we look at an athlete’s heart, at least to some extent. So is the enlargement we are seeing in a child due to: “normal” exercise at a competition level OR to the pathologic condition of HCM in its early stages??? An intolerably difficult question to answer.
We’ve found NO definitive test to make the decisions clearer. The best we can do is follow guidelines for: Left Ventricle (LV) dimension in diastole (> 55mm); LV filling (normal vs altered); family history (none vs positive); Maximal oxygen uptake (normal or increased vs decreased); and, LV wall thickness (> 13mm).
Any one of these things warrants further investigation, realizing that if we do find something we’ll know; but, if we don’t – we still don’t know for sure.
Commotio Cordis
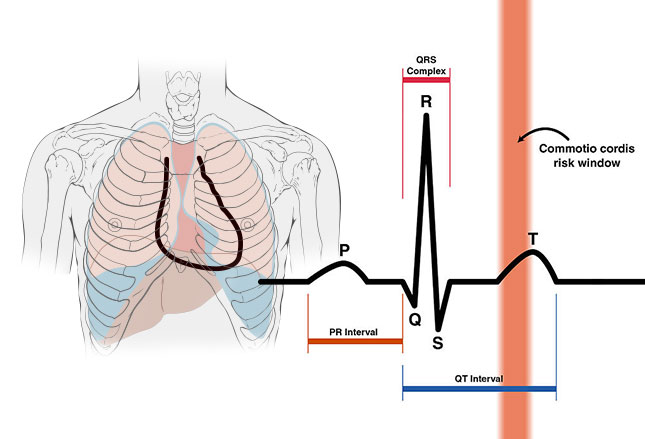
I’ve mentioned Commotio Cordis (CC) recently in another post. It’s a rare, but not unheard-of, incident where a person receives a strong blow to the chest just as their heart is “electrically” recovering from a beat: a puck, ball or helmet hitting square in the chest during the tiny 15-30 milliseconds at the start of a “T” wave (see graphic).
Most people know that striking the chest of a person can trigger a heartbeat. After all they show it on TV all the time. Well, an extra beat just when the heart has finished a normal beat is often just enough to trigger ventricular fibrillation – again, the stuff “heart attacks” are made of.
Young athletes are at increased risk for Commotio Cordis owing to the increased compliance (flexibility) of their chest walls. Unfortunately, chest protectors have not been shown to decrease an athlete’s risk of Commotio Cordis.
Pretty much every medical organization having anything to do with the heart recommends that all coaches, officials and parents be trained to recognize Commotio Cordis and what to do when it’s seen. That’s because it’s only seconds before SCA (arrest) becomes SCD (death) in a child.
We’ve learned a lot about the problem in the past 5 years even if we still can’t predict it. For example we now know that, if a child with CC is lucky enough to be resuscitated and live, we should undertake a complete cardiac evaluation to look for arrhythmias. And here’s the thing, IF no abnormality is detected, we can clear them to return to competition.
If possible, age appropriate safety equipment (e.g., safety baseballs) should be used and rules and coaching techniques should be adapted to limit chest contact.
ARVC Fatty Infiltration
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is an autosomal dominant genetic disorder common to the Veneto region of Italy. It’s where the right ventricle of the heart becomes infiltrated with fatty deposits. That, of course, enlarges it making it susceptible to fatal arrhythmia problems.
Like most everything else we’re discussing, the initial presentation of this condition is sudden cardiac death. But unlike others we’ve mention, about 30% of people with ARVC have a tiny change in their ECGs (epsilon waves) allowing us to “predict” possible events. Therefore, screening those with family members from the Veneto and family members of affected individuals is important.
Caffeine And Other Stimulants
Stimulants such as methylphenidate (shown), caffeine, pseudoephedrine and ephedra is EXTREMELY common among athletes at all levels of competition including childhood sports. AND, they have all been implicated in sudden cardiac death.
All of these increase heart rate and blood pressure over and above what exercise normally does, which places the child at risk for cardiac complications.
Caffeine may no longer be banned at low concentrations but it has many times been proven to negatively impact cardiac perfusion (blood to the heart muscle); even worse at altitude than at sea level.
Performance-Enhancing Drugs
Performance enhancing drugs (PEDs) are also commonly used by athletes, including children. A whole host of research has proven that PEDs (especially anabolic steroids) increase levels of cholesterol, VLDL, LDL and triglycerides as well as impact inflammatory markers.
That increase raises the person’s risk of coronary artery disease back to levels at least as great as the general population; so, completely negates any positive health benefit gained through exercise.
Preparticipation Cardiac Screening
To date (2016) the US has no “standard” protocol of screening tests for children participating in sports. Those over 40 years are screened when they start a new exercise program. European cardiologists, I’m told, do a “screening ecg on athletes of any age”; although, I’m not sure how that works for them.
Millions of children participate in sports in the US and screening every one with an ECG would not only be logistically a nightmare but extremely wasteful too. Perhaps over 99% of such exams would be “normal.”
Of course, we’ve already said that it’s prudent to screen those of Italian descent from the Veneto and those with a family history of heart disease. But that information is obtained in a good physical examination – which IS REQUIRED in most US children’s sports. That exam SHOULD ALSO CONTAIN the measuring of heart parameters before and after exercise – more important than an ECG for screening.
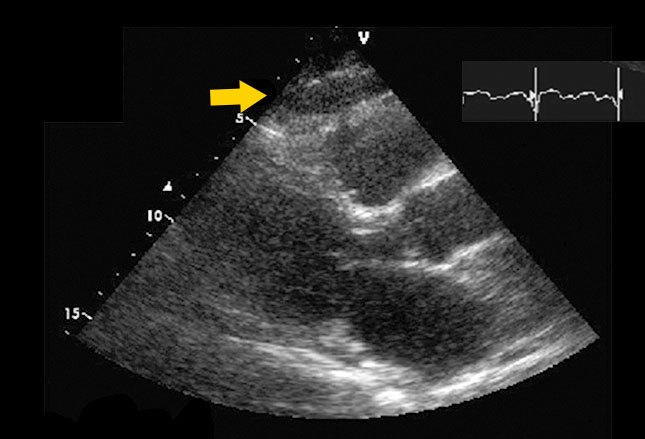
If any abnormalities are detected, an ECG can be done along with further evaluation and testing if warranted. The heart echo shown reveals epicardial fat over the free wall of the right ventricle (arrow).
CAD Exercise Testing
Just last year (2015) US heart associations recommended that any prospective athlete with coronary artery disease (known through ECG and other testing) should also undergo exercise testing. That is to make sure the amount of blood pumped is over 50% of normal and there’s no inducible ischemia – prior to “clearance” for an exercise program.
We also now make sure risk factor reduction changes are already in place and underway before clearing them for exercise.
Resuscitation
By definition, sudden cardiac death (the topic of this article) involves mortality; BUT, that diagnosis is not known until everything is over and certainly NOT made on the athletic field.
Until then everyone proceeds with the hope that the cardiac events we are seeing may be aborted with the proper and early treatment – which they sometimes are!
Coaches, trainers, parents and other first-responders need training to follow standard advanced cardiovascular life support (ACLS) protocols. And, although we don’t yet have much literature to document the successful use of defibrillators in resuscitating athletes who collapse, it is still recommended that automated external defibrillators (AEDs) be present at athletic events.
5 Posts in Child Cardiac Arrest (cardiacarrest) Series
- Commotio Cordis: Prevention and Return to Play – 9 Sep 2016
- Commotio Cordis: Treatment and Prevention – 26 Aug 2016
- Sudden cardiac arrest - case – 7 Aug 2016
- Sudden cardiac death – 26 Jul 2016
- Sudden Cardiac Arrest in a Child: Intro/Index – 25 Jul 2016