Tonsillectomy – Risks and Benefits
I have been asked several times this week about tonsillectomy – whether or not a child should have their tonsils taken out by surgery. Usually the question is in response to a sore throat of some kind, whether or not there is an infected tonsil.
There are just so many variables (i.e. whether it is acute or chronic, allergic or contagious etc.) that my reply must be largely individualized; so, a short article cannot adequately cover the topic.
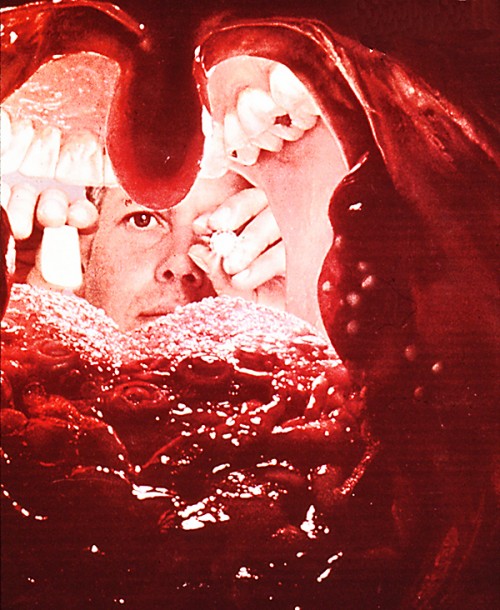
Tonsil eye viewThere are, however, some general concepts you should know about child tonsillitis treatment and tonsillectomy in particular.
Tonsillectomy Issues
The first issue is that a sore throat is either: pharyngitis (painful mucus tissues in the throat) OR tonsillitis (actually infected, tonsilar lymph tissues); AND that a tonsillectomy is never done for mere pharyngitis, even if it’s recurrent or in a child.
Approximately 750,000 Americans undergo tonsillectomy and adenoidectomy each year in the U.S., incurring costs approaching 1 billion dollars annually – a very lucrative procedure.
The tonsils are large lymph tissues on both sides of the opening to the throat. They are a part of a circle of lymph tissue, called Waldeyer’s ring, which surrounds the posterior throat, and aids in fighting off infection. Lymph tissue is the stuff that makes antibodies to fight away infections – and which make the body’s “disease memory” that prevents future infections. (The adenoids are also a part of this ring and will be discussed in a future article).
With the responsibilities of parenting, it is important to understand all the issues when someone (as well meaning as they may be) mentions to you “he sure seems to have a lot of sore throats,” or “aunt leona’s son had the same thing until he had his tonsils out.”
Second, you should be aware that tonsils perform an important function in fighting off throat infections. They become somewhat swollen with nearly every sore throat in a child. That’s their job and you can’t fault them for it.
Third, “infectious tonsillitis” is only one of the many causes of throats hurting. “Allergies”, actually are a more common cause, as they make the mucus which then drains down the back of the throat and causes irritation – Post Nasal Drip (PND). [And believe me, as far as a child’s pain is concerned, it’s often difficult to tell that PND is NOT a “real” infection.] Also, “Chronic Tonsillitis” is very rare, and most sore throats resolve using treatment with throat lozenges, salt water gargles and decongestants.
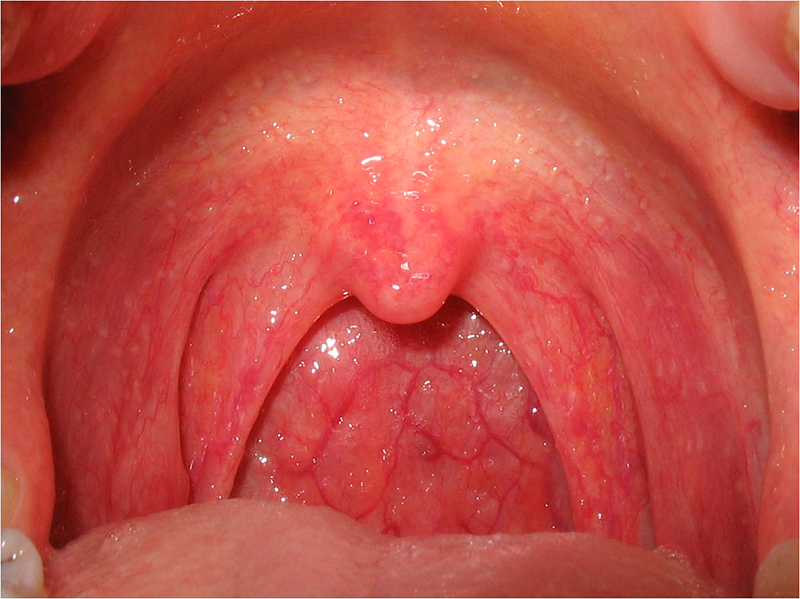 Normal teen throat, tonsils gone away
Normal teen throat, tonsils gone awayThird, the normal, healthy child has about one infection a month until he is ten years old — that’s almost one a month! Most of these are colds and sore throats — which, for a few years, are usually clustered one right after the other for months at a time in the winter.
Fifth, tonsils generally “melt away” to almost nothing as the child goes through adolescence. Sometimes, as they diminish, they form little pits and crevasses on their surface which can trap small pieces of food and produce bad breath – again, easily treated with throat lozenges and salt water gargles.
I have heard from more than a few parents that one surgeon in town tells his patients, after performing a tonsillectomy, “they were as big as a teenagers,” which, at best, is misleading. Commonly the teenage tonsils are the size of a bean – if that big.
Sixth, because of their causes listed above, the vast majority of sore throats are not caused by anything you can use antibiotics to treat (i.e. post nasal drip, allergies and viruses.)
And… last but by no means least… Seventh, tonsillectomy is not without risk! An analysis of 675,729 cases showed a mortality (DEATH RATE) of one child per 16,381 operations (0.006%). The same study showed a catastrophic hemorrhage (bleeding) rate of about 0.028%.
Not very large numbers, but when you talk about risking mortality (death), the operation had better be warranted for something more than mere snoring. Unfortunately, many are not!
Tonsillectomy Guidelines
So… what are the guidelines for the accepted indications for tonsillectomy?
1 — Cancer of the tonsil. This can occur in any age group. Biopsy of suspicious lesions are done first, followed by a tonsillectomy.
 Teen with exudative tonsillitis
Teen with exudative tonsillitis2 — Peritonsillar abscess. This is caused by a bacterial infection and the patient is usually very ill. Incision and drainage is mandatory to prevent extension of the infection into the space around the carotid artery.
About 8 to 10 percent of these abscesses recur and are much more cancerous the second time. Therefore, tonsillectomies are usually performed a few weeks after the individual has recovered.
3 — Congestive Heart Failure from airway obstruction by tonsils so large that a child has substantial loss of breathing ability (We are not talking about clogged nose, but a real “air gulper”).
This also goes for solid food dysphagia where the child’s tonsils are literally so large that it’s more than just difficult to swallow food – which would improve with growth and the normal dwindling of tonsilar tissues. Regurgitation of food, failure to thrive or significant weight loss could warrant tonsillectomy.
4 — The necessity of hospitalization to treat acute tonsillitis so severe that the child needs intravenous fluid and antibiotic therapy.
5 — Proven “strep” recurrent tonsillitis. It should be proven by throat culture to be caused by a certain type of “streptococcus.” Not just one or two infections but several which will put the child at risk for developing a heart condition known as rheumatic fever.
The tonsils usually come out after four or five episodes documented to be streptococcus.
Using the above criterion you can tell that there are very few tonsillectomies that should actually be performed.
There are some “philosophical indications,” however. Many physicians feel that a patient having four or more episodes of tonsillitis (not just pharyngitis – sore throat) a year, for at least two years and necessitating their missing ten or more days a year of school or work will benefit from a tonsillectomy.
However, these decision should be made in consultation between you and your child’s pediatrician.
It is probably better to discuss the case with, or ask for referral from, a pediatrician for a full physical exam and review of history prior to seeing an ENT specialist for the surgery.
2 Posts in Tonsillectomy (tonsillectomy) Series
- follow-up and clarification – 25 Apr 2015
- Indications for surgery – 21 Apr 2015
Advertisement by Google
(sorry, only few pages have ads)