Treating Fever in Infants, Children and Teens
If other pediatricians are like I am, one of the most common topics they discuss on the phone is fever.
Callers sometimes simply state, “My baby has a fever” or “John has a fever of 103” or “Sally has a fever again; she needs some antibiotics,” – as if fever were the disease.
Fever can be a problem, but not for the reasons implied in the above statements.
Many people are surprised to find that fever can be helpful in fighting off illnesses. Let’s discuss some of the facts and myths about fever.
First: Fever is not an illness or disease in itself. It merely represents the body’s active defense mechanism toward another illness.
As some bacteria and viruses produce their infections, they release compounds known as pyrogens. These substances cause the body to produce fever.
In addition, as the body’s own blood cells fight off infections, they too release some similar pyrogens.
Studies have shown that the body fights off infections better, and viruses don’t grow as well, at slightly higher than normal body temperatures.
 Second: There is a difference between fever and temperature.
Second: There is a difference between fever and temperature.
Normally, temperatures within a child range from 97.7°F (36.5°C) to 99.5°F (37.5°C) in the mouth, 98.6°F (37°C) being what we call “normal.” However things like exercising, wearing too many clothes, taking a hot bath, or being outside in hot weather can easily cause it to rise to 100.4°F (38°C) and still not be called a “fever.”
The “normal” range for rectal temperature is higher, the “normal” range for axillary temperatures is lower. Axillary, ear, and forehead temperature measurements are easier to obtain than rectal or oral temperatures, but they are less accurate and may need to be confirmed rectally or orally in certain children.
So, when is a temperature considered a “fever”? Well, there is really no single value that is defined as fever. However, the following are generally accepted values:
◾Rectal temperature above 100.4ºF (38ºC)
◾Oral temperature above 100ºF (37.8ºC)
◾Axillary (armpit) temperature above 99ºF (37.2ºC)
◾Ear (tympanic membrane) temperature above 100.4ºF (38ºC) in rectal mode or 99.5ºF (37.5ºC) in oral mode
◾Forehead (temporal artery) temperature above 100.4ºF (38ºC)
 Third: The degree of fever has very little to do with the degree of illness. A higher temperature does not mean the child is more sick.
Third: The degree of fever has very little to do with the degree of illness. A higher temperature does not mean the child is more sick.
Physicians have all seen many children with 105 temperature running around playing as if nothing was wrong, and similarly children with a low-grade fever in intensive care.
It’s not the fever that counts so much as the other symptoms. That’s what you should watch for and report to your doctor.
Fourth: Fever does not mean that antibiotics are needed.
In most all illnesses, even viruses, the fever is the first sign to appear. It should merely alert both parents and doctors to watch the child more closely over the next few hours/days for the development of other symptoms of illness.
 If the child is seen by the doctor too soon after the onset of fever, the site of infection might not be apparent.
If the child is seen by the doctor too soon after the onset of fever, the site of infection might not be apparent.
Therefore, if the child is over three months old, is fairly playful and is eating, with no other symptoms (like stiff neck, severe abdominal pains, seizure, difficulty breathing — more than nasal congestion, etc.) it might be wise to observe for a day and allow the rest of the symptoms to develop.
If the illness is caused by a bacteria, then your physician will institute antibiotic therapy. This will not treat the fever specifically, but will treat the underlying disease thereby making the fever go down – which is the way we want to do it.
Fifth: Fever does not even mean that it should be treated. A child older than three months who has a rectal temperature less than 102ºF (38.9ºC) and who is otherwise healthy and acting normally does not require treatment for fever.
Children who have underlying medical problems, including diseases of the heart, lung, brain, or nervous system are the ones you should consider giving treatment to their fevers. In children who have had febrile seizures in the past, treatment of fever has not been shown to prevent seizures, but is still a reasonable precaution.
 And sixth: Seizures are almost never caused by an existing high fever, but rather by a temperature that goes up rapidly or comes down rapidly in a child who is prone to them.
And sixth: Seizures are almost never caused by an existing high fever, but rather by a temperature that goes up rapidly or comes down rapidly in a child who is prone to them.
If your child feels warm and you find that he already has 103 temperature by the time you take it, the major risk of febrile seizure has already passed.
I hope by now I have allayed most fears about fever. There are, however, some problems associated with fever.
Infants who are less than three months of age who have a rectal temperature of 100.4ºF (38ºC) or greater, regardless of how the infant appears should be evaluated. Especially newborns under 8 weeks of age. This is because infants, as yet, have a poorly developed immunity system, and infections can spread very rapidly.
Also, fever does make a child somewhat tired, feel "sick", and sweat more. Therefore he needs more liquids to replace body fluids lost.
Some general guidelines to treat fever would be as follows:
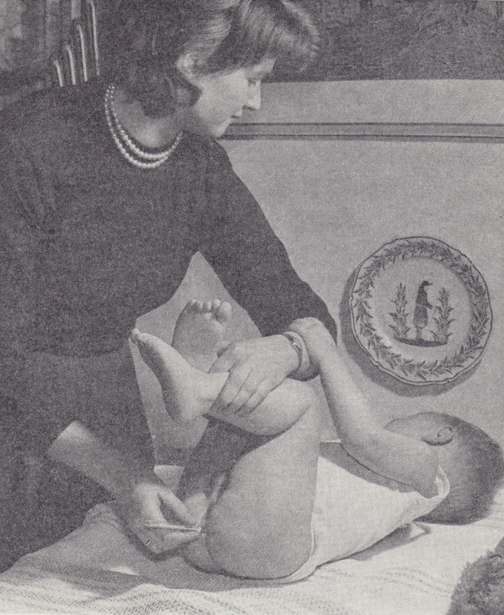
- The first treatment should always be to unclothe the child. Leave the child in a diaper or under shorts until the fever drops and then a light cotton sheet. The most common reason for medicines not to “work” is because the child is over bundled.
- Medicines are best reserved for children with temperatures above 102ºF rectally.
- Encourage fluids. Don’t force solids or milk if a child’s not interested.
- Antipyretics (anti-fever) medicines like acetominophen (Tempra, Tylenol etc.) or aspirin can be given every four hours. Follow the dosage schedule given on the package of the particular medicine you buy. Neither medicine should be given more frequently than every four hours, and only in the correct doses.
- If child’s fever remains after the above methods, and there aren’t any other symptoms, sponging with lukewarm water will reduce the temperature, but may not in the long run help the child.
When To See A Doctor
◾Infants who are less than three months of age who have a rectal temperature of 100.4ºF (38ºC) or greater, regardless of how the infant appears (eg, even well-appearing young infants should be evaluated).
 ◾Children who are three months to three years who have a rectal temperature of 100.4ºF (38ºC) or greater for more than three days OR who appear ill (eg, fussy, clingy, refusing to drink fluids).
◾Children who are three months to three years who have a rectal temperature of 100.4ºF (38ºC) or greater for more than three days OR who appear ill (eg, fussy, clingy, refusing to drink fluids).
◾Children who are 3 to 36 months who have a rectal temperature of 102ºF (38.9ºC) or greater.
◾Children of any age whose oral, rectal, tympanic membrane, or forehead temperature is 104ºF (40ºC) or greater or whose axillary temperature is 103ºF (39.4ºC) or greater.
◾Children of any age who have a febrile seizure. Febrile seizures are convulsions that occur when a child (between six months and six years of age) has a temperature greater than 100.4º F (38ºC).
◾Children of any age who have recurrent fevers for more than seven days, even if the fevers last only a few hours.
◾Children of any age who have a fever and have a chronic medical problem such as heart disease, cancer, lupus, or sickle cell anemia.
◾Children who have a fever as well as a new skin rash
◾Children whose fever is fairly unremitting for three days even though no new symptoms develop can be checked in the office.
Above all, use common sense. You know your child best.
If you feel he should be checked, get medical attention. If fever is the only symptom, take appropriate action at home and see medical care as needed.
Advertisement by Google
(sorry, only few pages have ads)