Virginia Apgar: Blue Babies
I think I’ve said something like this before but today’s number 45 of the top 50 physicians making a lasting impact on the field of medicine is known by EVERY pediatrician in the world, and most other physicians too. But that’s the definition of “lasting impact” isn’t it.
In 1949 Dr. Virginia Apgar was the first female full professor at the Columbia University College of Physicians and Surgeons and in 1953 went on to create what became known as the “Apgar score.”
Dr Virginia Apgar, pioneer in pediatric medicine
Virginia Apgar (1909-1974) – #45
Cultured, Determined, Gentle Giant of Medicine
That meant I was born several years BEFORE there was any standardization in medical parlance to describe a baby’s physical condition at birth. An extremely risky place to be because that meant there was no way to tell what effect the delivering doctor’s “heavy hands” or “techniques” contributed to the “well” or “ill-being” of the infants they were delivering.
That’s what we call the “lack of evidence-based medicine.” Now days we use evidence-based medicine which means that we put specific standardized measurements in place and use them to tell whether or not what we do makes any difference (or sense.) It also helps the comparison between different researchers.
Dr. Apgar’s scoring method was the first standardized tool to evaluate a newborn and has become the “gold standard” – still used today – in evaluating generations of “stunned” infants newly welcomed into the “outside world.” This single “invention” has saved millions of babies around the world and probably will save millions in the future.
Early Life and Education of Virginia Apgar
But let’s start at the beginning. She was born, the youngest of three children, in Westfield, New Jersey on 7 june 1909 to a music-loving family with a businessman father having an inherent love for all things science especially inventing equipment involving electricity and radio waves in his basement lab.
But with Virginia the ‘beginning’ began in high school. Her father’s incessant scientific hobbies, her oldest brother dying from Tuberculosis and another having a chronic illness – Virginia left high school with the determination to be a doctor and nothing stood in her way.
Scholarships helped her attend Mt. Holyoke College where she was a noted and gifted violinist and cellist and in 1929 graduated with a major in zoology and minors in physiology and chemistry.
She entered the College of Physicians and Surgeons at Columbia University in September 1929 – and Wall Street did its historical crash in October. Despite needing to do odd-jobs to survive she graduated fourth in her class in 1933.
Then absolutely determined to be a surgeon, she won a surgical internship at Columbia and performed brilliantly; However, the chair of surgery (Alan Whipple) counseled her about changing goals.
He described other women he had trained in surgery who had failed to establish successful careers and pointed out his observation that her beloved field of surgery couldn’t advance until many improvements were made in anesthesia (back then mostly handled by nurses and not a medical specialty). He told her she had “the energy, intelligence and ability needed to make significant contributions to the specialty.”
Fortunately for us all, she decided to take his advice (instead of the then burgeoning method of the feminists to plow ahead protesting the inequality); but, anesthesiology wouldn’t be recognized as a specialty until the ’40s so she had no place to train when she finished residency in 1937.
She ‘took two steps backward’ a bit and studied in other institutions in order to obtain a ‘certificate’ in anesthesiology which was the ‘required’ entrance portal to the world of anesthesiology.
Medical Career of Virginia Apgar
In 1938 she returned to Columbia as director of the new division of anesthesia and as an attending anesthetist; but, because of prejudice in the male dominated profession of surgery couldn’t recruit other doctors to work for her.
She was a ‘department of one’ with little funding or support until she and many of her co-workers threatened to quit Columbia; which did get her funding and attention for the department. In 1949, when anesthesia became an academic department, she was passed over for a man as chairman but was appointed the first woman full professor at the school.
Now responsible for officially-accepted research she knew that no such thing could be done without some way to measure clinical condition of the neonate and used her many years of observations to ‘change the world’ as it would turn out. At that time anesthesia was being given to mothers in labor to assist them through the process; which, she had observed was not without its consequences to the baby.
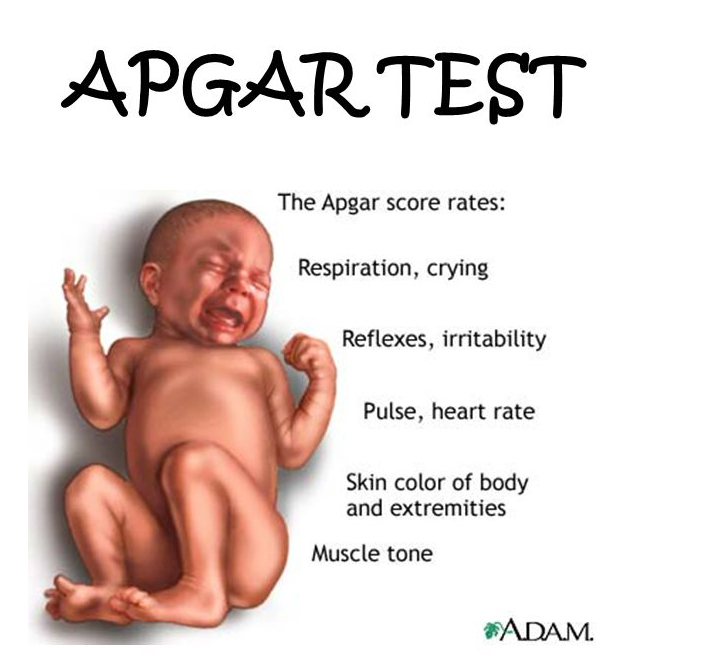
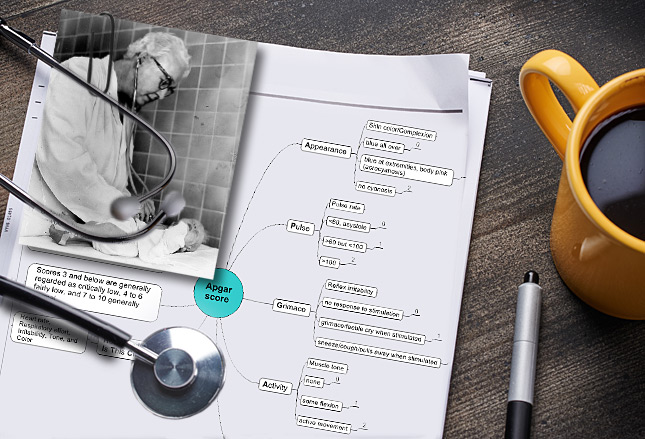
At one minute after birth, babies could be classified on five observations in order to tell whether they needed to be resuscitated from the effects of the mothers anesthesia: heart rate, respiratory effort, muscle tone, reflex response and color. All five were given a score of 0, 1 or 2 and that total determined what should be done.
This score was presented in a national meeting in 1952, published in 1953 and slowly began to revolutionize the specialties of Obstetrics, Surgery, Anesthesiology and Pediatrics! Now all the varied approaches to care of mothers and babies became visible for all to see and babies were saved.
Ten 10 years later other doctors created a pneumonic, to aid in remembering it, known as the A.P.G.A.R. score:
Eventually, other measurements were factored in to discover that a common anesthetic (cyclopropane) was good for mothers but bad for babies and produced highly acidic and low oxygenated blood. That changed medicine!
Then, if one measurement at 1 minute was good, more were better and others began taking them at all different times. A twelve-hospital study of 17,221 babies established definitively that the APGAR score, at one and five minutes, predicted not only a babies survival of birth but its subsequent neurological development as well!
One and five minute scores were found most meaningful and are still used today. One for the effects of pre-birth treatment and five for how well the post-birth resuscitation was doing. Every one of you born after 1953 has received TWO APGAR score’s – whether you knew it or not!
Public Career
After her struggles she took a sabbatical leave from Columbia in 1959 but instead of resting she earned a master’s degree in public health from Johns Hopkins and decided not to return to academic medicine.
Instead she wrote many articles and essays, traveled, spoke; always traveling with her violin and playing in amateur chamber quartets wherever she happened to be. A friend introduced her to instrument-making and together they made two violins, a viola and a cello.
She was an enthusiastic about gardening, and enjoyed fly-fishing, golfing, and stamp collecting. In her fifties, she started taking flying lessons, stating that her goal was to someday “fly under New York’s George Washington Bridge.”
She was asked, on many occasions, to join or take part in women’s organizations and causes but for the most part avoided them insisting that “women are liberated from the time they leave the womb.”
Retiring from academia she began working on behalf of the March of Dimes Foundation and not only became vice-president and director of basic research for them; but, also altered their course toward treating and preventing birth defects. She alerted them to the problems of premature birth, which is now one of their top priorities.
During the pandemic of 1964-65, she became an outspoken advocate for universal vaccination to prevent mother-to-child transmission of rubella resulting in 12.5 million cases, 11,000 miscarriages or abortions and 20,000 cases of congenital rubella.
She traveled thousands of miles each year to speak to widely varied audiences, including teens, about unwanted pregnancies and the importance of early detection of birth defects. She wrote the 1972 book “Is My Baby All Right?” with a co-author and eventually became a clinical professor at Cornell teaching teratology (birth defects) in the pediatrics department.
The American Academy of Pediatrics founded a prize in her name and she received numerous awards from medical associations, colleges and societies – all the way from honorary doctorates to “Woman of the Year” by the Ladies Home Journal.
Virginia never married, and died of cirrhosis of the liver on August 7, 1974 at Columbia-Presbyterian Medical Center. She is buried at Fairview Cemetery in Westfield.
Biographic Summary
Virgina Apgar was an invaluable asset to medical history by developing an entire branch of medicine, anesthesiology, and saving countless newborns with her APGAR Score.
Born: 7 June 1909, Westfield, New Jersey
Died: August 7, 1974, Columbia-Presbyterian Medical Center; interred at Fairview Cemetery in Westfield.
Education: BS at Mt. Holyoke College, 1929; MD and Surgical Residency at College of Physicians and Surgeons at Columbia University, 1933 and 1937.
Known for: Development of Anesthesiology as a branch of medicine, invention of the APGAR Score which revolutionized newborn care and research
Books: Is My Baby All Right, 1972 with co-author.
26 Posts in Top 50 Doctors (top50) Series
- 26 - Carlos Chagas, Chaga's Disease & pneumocystis pneumonia. – 10 Apr 2025
- 27 - Charles D. Kelman - Cataracts – 9 Mar 2023
- 28 - Cicely D. Williams, Kwashiorkor, Breastfeeding, Whistleblower – 21 Jun 2022
- 29 - Dame Cicely Saunders, Hospice – 23 Apr 2018
- 30 - David L. Sackett, Evidence-based Medicine – 2 Apr 2018
- 31 - E. Donnall Thomas & Joseph Murray, Bone Marrow Transplants – 23 Feb 2018
- 32 - Elizabeth Blackwell, women in medicine – 29 Jan 2018
- 33 - Elisabeth Kübler-Ross, stages of grief – 5 Jan 2018
- 34 - Watson & Crick, DNA – 2 Dec 2017
- 35 - Mahmut Gazi Yaşargil, Micro-Surgery – 24 Oct 2017
- 36 - George Papanicolaou, Cytopathology, Cancer – 29 Sep 2017
- 37 - Dr. James Parkinson, Parkinson's Disease – 1 Sep 2017
- 38 - Dr. John Snow, cholera – 20 Aug 2017
- 39 - Dr. Joseph Kirsner, GI Joe – 27 Jul 2017
- 40 - Lawrence (Larry) Einhorn, chemotherapy – 16 Jun 2017
- 41 - Robert Koch, modern bacteriology – 21 Mar 2017
- 42 - Stanley Dudrick, TPN – 28 Feb 2017
- 43 - Stanley Prusiner, neurodegenerative diseases – 25 Jan 2017
- 44 - Victor McKusick, medical genetics – 3 Jan 2017
- 45 - Virginia Apgar, anesthesiology & newborn care – 12 Nov 2016
- 46 - William Harvey, circulation – 12 Oct 2016
- 47 - Zora Janžekovič, burns – 26 Sep 2016
- 48 - Helen Taussig, blue babies – 3 Sep 2016
- 49 - Henry Gray, anatomy – 3 Jul 2016
- 50 - Nikolay Pirogov, field surgery – 11 Jun 2016
- Top 50 Doctors: Intro/Index – 10 Jun 2016

