Yogi Berra’s Tips For Practicing Medicine and Parenthood
I’m going to take a stab at a posting about another doctor’s observations which seem to have struck me strongly enough that they’ve captured much of my mental “wait cycles” over the past week. You know, the “cycles” of your fast mental computer where it’s “waiting” for other things to “catch up” so it can move on.
Some people call it “time-sharing your brain” others just “day dreaming.”
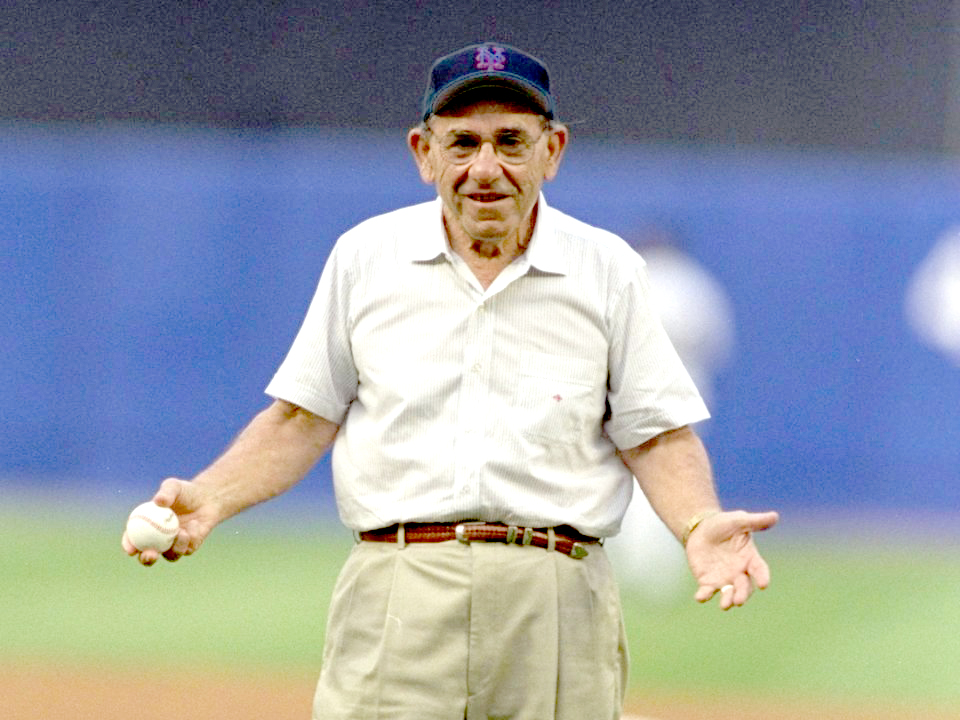
Baseball Hall of Famer, Yogi Berra
Actually, it’s two people I’ve been musing about: Dr. Julian Seifter and Lawrence Peter Berra – the Baseball Hall of Fame-er and quipster, more commonly known as “Yogi” for short.
Seifter wrote an article where he tried to apply Yogi’s baseball quips to his practice of medicine; but, it seemed to me that he left some good ones out and he didn’t even touch on how Yogi’s heuristics represent patient’s.
So many personal experiences came to mind while reading his article that I placed it in my “future draft” pile and it’s finally come to the daylight: Yogi Berra’s Tips.
Yogi Berra’s Tips on Being A Doctor and Being a Patient
A heuristic is something we use, like a plan or an algorithm, which helps us wade through complicated things faster – like a shortcut. Yogi, perhaps without knowing he was doing it, just seemed to come out with a lot of them.
On first reading, you might need to shake your head and say “Huh?” But then the thing sorta just settles in and clicks and you realize he’d just said an entire paragraph in a simple sentence, usually with two or more meanings and a whole lot of applicability to the human dilemma.
I was playin’ American Legion Baseball. Bobby Hofman (used to play with the Giants) and I were on the same team. We never had dugouts. We’re sittin’ on the ground. I always had my legs crossed and my arms folded. Bobby said, “You look like a yogi.” And it stuck.
Because a physician’s (and patient’s) world is every bit as prone to mishaps and chance as is baseball, many of Yogi’s sentiments have application to us too. Here are a few:
“When You Come to a Fork in the Road, Take It”
Decisions are part of the normal human dilemma for both doctors and patients. In medicine decision carries with it much more weight… and consequences.
While indecision may put things merely “on hold” or go away entirely in other aspects of life; in medicine it often leads to continued and more invasive testing and expense OR someone or something making the decision for us… not always for the good.
We order tests and expect some definitive answer for the patient. If they are not conclusive, we order more and then more, hoping that we don’t end up no better off than we started with. Lack of clarity and commitment from lab and consultants is not helpful to a clinician; deliberate waffling is costly and wasteful and increases the chance of error.
I’ve ordered xrays in the past and had the radiologist send back a report where he merely parroted back my own words to him exactly, as if he was taking credit for them, in his “impressions.” Dr. Seifter described sending to the lab a tiny (possibly inadequate but VERY difficult to obtain and unrepeatable) kidney biopsy and finding that his pathologist had done just the opposite.
He had made extraordinary effort and took “one half of a glomerulus, performed morphometrics, and determined that it had a thin basement membrane consistent with hereditary nephritis … (and had the professionalism to) give his professional opinion. Thus,” Seifter bragged, “although I had a poor sample, I had a good pathologist.”
Making a decision without adequate information or “omniscience” is terribly difficult; not making any decision at all is often terribly foolish.
Says Dr. Seifter (and me): “A good clinician/parent is willing to make a decision and stand by it. Over time, it becomes apparent whether that clinician/parent has good judgment – which is the best skill anyone could have.”
Those forks in the road? Take them
“We Made Too Many Wrong Mistakes”
There are “right” mistakes you know (for want of a better term). Those are the ones completely unexpected which lead to better understanding, invention and learning. WRONG mistakes are those you’ve already made once before but didn’t learn from or caused yourself through laziness, incompetence or neglect.
In medicine it can also occur when you’ve already made a mistake (at diagnosis) and either through stubbornness or traits I just listed hold to it without question, thereby causing further damage or delay in treatment.
In my medical school days we called it “the old chart will come back to haunt you” – meaning that if someone in the past (wrongly) interpreted a rash as measles then everyone during the next seven admissions for the same thing wouldn’t even consider (or look for) the real diagnosis: tertiary syphilis. That meant the poor child who had been abused was now sitting in the wrong hospital ward being exposed to REAL measles!
It’s called “anchoring” or “confirmation bias” and it haunts us all and leads to lots of needless patient suffering. Dr. Seifter told of a patient diagnosed with a paranoid schizophrenia when he rotated through psychiatry service, who they eventually found actually to have neurosyphilis, which could have been treated with penicillin.
And we all have such stories: mine was sitting in daily rounds and listening to the teaching staff praise the resident covering the pediatric ward for a week (for his handling of a tough child abuse case); before taking over from him and finding (through completion/repetition of key diagnostic tests) that the child’s diagnosis was really Henoch-Schonlein Purpura which was causing the bruising – just like the parents had been frustratedly trying to convince the police the whole time.
Mast cell disease and other difficult-to-diagnose conditions, such as fibromyalgia, often involve years of chronic debility without effective treatment because of the persistence of “wrong mistakes.”
Morale: sometimes the chance that you are wrong is in direct proportion to the strength you are trying to prove yourself right.
“You Can Observe a Lot by Just Watching”
This one I’ve learned several different ways, from more than one teacher and under multiple circumstances. The first was from a sinewy, high-strung professor of neonatology at the University of California in San Francisco. I grew to respect him, despite his many idiosyncrasies.
His favorite expression, especially to new residents, was: “$%! $%*@ it! You’re killing this kid!” Right before he taught you ANYTHING – from bandages to fluid management. However another of his favorites was “I believe in the hover philosophy.” If we didn’t know what was going on with the infant he wanted us to “hover” over them until we discovered the problem. Literally. No kidding. And we all saw him do it too.
Sometimes that meant looking over the nurses shoulder for an hour or two or three, changing diapers, drawing blood ourselves, doing a feeding – literally whatever it took until we DID see the problem… and I’m here to tell you, it works! I’ve done it many times, and still do.
Just because we CAN do something it doesn’t mean that we SHOULD do it.
Dr. Seifter’s article described a patient who was sent for a fairly innocuous vaginal ultrasound because the doctor felt a mass during a routine gynecologic visit. Didn’t find a mass on the ultrasound BUT a possible renal cystic lesion was mentioned on the report; so, next a renal CT scan was done. It showed a ureteropelvic obstruction that the patient had from birth with well-preserved renal tissue and no necessity to perform further testing.
HOWEVER, some ambiguous sort of “cystic lesion” was noted on the report to have been seen over on the pancreas side of things; so, you guessed it – pancreatic MRI with a fairly invasive sampling for cytology.
“It was all negative,” Seifter reported, “but in between the diagnostic testing was a world of unnecessary worry.”
Personally, I still have the emotional scars from the several times I’ve seen a child with a fairly high fever, watchfully waited at home with OTC fever medicines until I couldn’t stand it any more and admitted them to the hospital for lumbar puncture and possible antibiotics only to have it finally break on its own when blisters broke out in the child’s mouth: primary herpes stomatitis. No need for antibiotics, further testing or hospitalization.
Sometimes an unrelenting hundred and four temperature that is making the child miserable and the parents clearly panicked and doesn’t respond to anything you do for 6 or 7 days is an excruciatingly difficult situation to endure for a physician – not to mention what it does to the parents – even if you camp out at the hospital and diligently watch for any sign of any other problem.
Watchful waiting – non-intervention – can sometimes be the most effective intervention.
All physician’s have a mantra taught to them in medical school. In latin it’s: primum non nocere – “first do no harm” in English. That can mean sometimes that the best treatment is “no treatment.”
“Fifty Percent of Baseball Is 90% Mental”
This Yogi-ism takes some pondering and just when you think you get it you realize you probably don’t. I’m sure he was trying to allude to the psychological aspect of learning and playing the game. That’s true in medicine as well – probably even more so; and it’s true in being a patient, a parent, a child and just about everything else too.
On this I think Dr. Seifter pretty well sums it up for both of us.
“There is more to an illness than just the illness; how people fare often has a lot to do with their reactions to the illness. There are patients who are ‘not sick’ – the deniers who deal with their illness by trying to wish it away; or, those who are ‘too sick’ – they are so obsessed with their disease that they are completely controlled by it.
The ones who do best are, like Goldilocks, ‘just sick enough’: They acknowledge the illness, but they also put it aside at times in order to make room for living.”
“We Sure Are Lost, but We’re Making Good Time”
Back in the days of regular manned space events it used to be in vogue to tell aeronautic jokes. One was about a janitor overhearing a group of airplane designers arguing over the best way to prevent a new aircraft’s wings from routinely and spontaneously ripping off in the air once it’s velocity got to a certain speed.
He startled all of them into silence by matter-of-factly stating: “if’n it were me, I’d put some holes along where it tears” then left the room before they had a chance to question, rebut or mock. They all had many clear reasons why the idea was complete foolishness but one decided to try it out on a model in a wind tunnel and it worked great! No loss of wings or plummeting to the ground.
The next day they cornered the guy and demanded to know how he knew such a thing would work. With the same aplomb and confidence he merely continued his dusting and said: “Don’t ask me, I just know that toilet paper never tears on the perforations.”
Why do we do the things we do, the way we do them? The truth be told and we’re being honest with ourselves, mostly because we’ve just noticed that they work. Simple as that.
In the entire history of modern medicine before Obama, with his brand of socialized medicine and multitude of mandated presidential directives, there’s never been a time where guidelines, efficiency, and emphasis on the handoff and the discharge of patients more ruled our medical behavior – or when understanding was increasingly more irrelevant!
We’ve already described “anchoring” and how an early wrong decision cascades into more and more deadly wrong turns. The so-called “electronic medical record” (EMR) has demonstrated that it can not only exponentiate serious errors but enshrine and perpetuate them as well – much more than paper-pulp and graphite ever could.
More and more the “computer thing” in the exam room takes on it’s own life which defies normal methods of deleting and editing; and we can now make mistakes at the speed of electrons!
Again, Seifter takes the words right out of my mouth: “Some of clinical practice – a lot, really – is guesswork, a heuristic, a shortcut, a sound bite, but we begin to mistake our habits for the truth.
There is confusion between truth and custom. And sometimes the emphasis is on following the rules and performing the procedure rather than on ultimate outcomes. ‘The operation was a success, but the patient died.'”
Although, like Yogi says: “we’re making good time.”
“I Never Make Predictions, Particularly About The Future”
Patients and TV dramas want us to do it all the time: What’s the prognosis doctor? A prognosis is just the medical word for a prediction and in medicine it ALWAYS comes with an entire boatload of assumptions and caveats.
“Well,” we have to say, “IF the patient’s course is within 1 standard deviation of the possible mean outcomes AND the treatment acts like the majority of times we use it AND there are no other complicating factors AND our diagnosis is correct in the first place AND … the computer network doesn’t go down THEN it’ll probably be thus-and-such — give or take.”
Despite what the bureaucrats want everyone to believe and how they act, regulations, rules, treatment algorithms and policy mandates are not always applicable to a particular individual – a patient has the inalienable right to be an exception to the rule and we just have to get over it and move on.
We like it to be “déjà vu all over again” whenever we diagnose and treat an illness; but, it rarely is. Sometimes patients like to “Pair up in threes” and follow their own course.
“In theory there is no difference between theory and practice; [but] In practice there is” which is why we need to know when to hold off on treatment or modify it if our first effort is not working like predicted. “If the world was perfect, it wouldn’t be.”
We may use guidelines and evidence to initiate treatment due to the fact that “you’ve got to be very careful if you don’t know where you are going, because you might not get there.” However, there is a lot of uncertainty in what we do and we often have to “Take it with a grin of salt” and adapt new treatments – “the future ain’t what it used to be.” How can it be? “Now” isn’t the same as it was either!
As physicians we should be humble in our pronouncements and encouraging of the future. Remember: “It ain’t the heat, it’s the humility” – and there’s a lot of that required these days.
Yogi said “I never said most of the things I said” and perhaps he was overzealously quoted sometimes; but, we loved the guy and we wanted him to have said them. He died at 90. He was a sports figure of my youth and “a nickel ain’t worth a dime anymore.”
One thing he DID say however was that “Little League baseball is a very good thing because it keeps the parents off the streets.” Ain’t it the truth!