Bed Wetting (Enuresis) — Part 2
Last week I described the problem of enuresis (bed wetting) — how it is fairly common (10-20 percent of seven year olds) and how there are a large number of contributing factors.
I have recently become aware of the statistic that approximately 3 percent of marine corps inductees have wet the bed within a year prior to their induction.
Bed Wetting is Enuresis
The contributing factors to bed wetting are, for the most part, initially beyond the control of the child and are therefore not punishable offenses; however, motivation should be there — so that when the child is physically capable of being dry, sheer force of habit does not prolong the problem unduly. There should be no undue coercion or punishment.
Watching for this "readiness" time, while minimizing the damaging effects that enuresis has on the child’s self-esteem, is the real goal.
 This problem really should be evaluated first by a pediatrician who sees chronic problems. It is infrequent that a referral to a urinary specialist is needed.
This problem really should be evaluated first by a pediatrician who sees chronic problems. It is infrequent that a referral to a urinary specialist is needed.
You should be aware, however, that in this problem there is a wide variation between doctors in the amount of workup and time spent in the office educating about the problem. Some do it well others don’t take much interest in it.
It should not be a rushed “by the way, Johnny wets the bed” type of visit. Ask for an extended appointment. Get a baby sitter for any other children and don’t take anyone else but the patient with you. And when you’re there don’t talk about any other problems but the bed-wetting.
There is a difference between issues which are “uncommon” and those which are “normal.” Certainly the percentage of children who have it isn’t high enough that I would call it “normal” for a ten-year-old. But, just because we call something “not uncommon” doesn’t mean that we should be so blasé that we don’t do a thorough enough physical exam to be able to rule out other problems – many of which are more significant and treated much differently.
Expensive laboratory studies are usually not indicated, at least initially. What is needed is the physician’s time— time to take a thorough history and do a complete head-to-toe examination – time also to explain, teach and counsel, and more time to follow up.
Treatment Methods
The basic elements of treatment (preferably in this order) will probably be:
- Self-responsibility. Although the child can’t usually help it, it nonetheless is his/her problem and really no one else’s. Mothers are angry; father’s either deny or are embarrassed; siblings tease and taunt; and the child is depressed and anxious.
Within the limits of his ability, the child can take total responsibility of the problem — changing bed, washing clothes and sheets, having own bath, taking own medicine, etc., without coercion or belittlement. - Bathing every morning. Urine has almost no odor, until bacteria have worked on it changing it to ammonia. Therefore, if clothes and bed clothes are washed every day, a protective mattress is used and kept clean and the child bathes in the morning, there is little need for the other children at school to even know, much less tease about it.
- Minimize drinking liquids for two hours prior to bedtime. A small drink two hours prior to bedtime frequently controls the child’s thirst. Parents may want to briefly awaken and take the child to the bathroom when they go to bed themselves.
- Eliminate food allergens. Stop any food which has in the past (even in infancy) caused food allergies, for a month’s trial period. Also, caffeine containing drinks (yes even soft drinks) drunk any time in the day can influence enuresis both through bladder sensitivity and overall nervousness.
- Attempts at decreasing anxiety. Anything that increases anxiety in a child’s life should be sought out and dealt with. Emotional conflict, anxiety, parental problems, etc., and even life style habits.
In my counseling I have seen everything from hard rock-and-roll music to unrestrained use of HBO with inappropriate movies, to frequent masturbation, to family arguments, to death threats at school, and many others affect or even precipitate the anxiety that reinstitutes the child’s enuresis.
[This is one time where the adage “you don’t find out unless you ask” really holds true. And a doctor asking the questions, if they will, frequently obtains different answers than those parents receive.]
I recommend no TV during the hour prior to bedtime; but, instead, soft, soothing reading type music, and a quiet time with mom or dad each night. - A discrete star chart. There should be five or six stars possible for every day — one for being dry, but all of the rest should be under the child’s conscious control (like washing own clothes, remembering no fluids, cleaning room, etc.).
Unless the child is very young, the chart should NOT be kept where the whole world can see it.
Rewards should be tailored to each child and should be designed to provide daily motivation as well as weekly.
Rewards should be specific for the child and should not involve any other member of the family. The last thing he needs is to have the family on his case because they didn’t get to go to the show. - Bladder stretching exercises probably don’t hurt, even if they might be a bit “academic.” Each day the child tries to hold his urine as long as he can and then voids (urinates) into a measuring container – expecting that there will be slight increases over time.
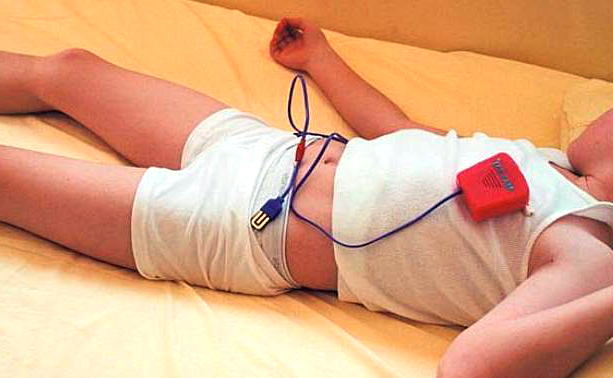
As the amount is recorded on the calendar, over a period of time there should be a gradual increase the amount of urine that can be contained in the bladder; which, might translate to longer times between needing to void even at night. - A wetting alarm may be used on the older child to use operant conditioning to train him to be sensitive to the "signals" coming from his full bladder. The best kind is the one in which the snaps fit right on the child’s underwear. The wire extends up to an alarm, worn like a watch on the child’s wrist. And it’s LOUD!
The training is being done into the subconscious and, therefore, does not happen quickly. Over several weeks to months, the child gradually learns to wake up and go to the bathroom during the night if needed.
But they MUST get up! Many will be "too tired" and some even lay there and let the alarm ring. Parents should start the child out correctly for the first couple of weeks; hearing the alarm and making sure that he awakens, goes to the bathroom, changes clothing and sheets and re-sets the alarm before going back to bed.Most children will tell you that waking up is preferable to having a wet bed!
- Medication may be used in the older child on an individual basis. The medication, Tofranil, seems to work by causing a small degree of urinary retention and possibly decreasing the amount of dream sleep. It is extremely deadly when taken in a poisoning dosage, especially to younger brothers an sisters.
- Pituitary hormone, although more readily available now, should never be used for this minor condition.
- I’ve seen Hypnosis work when the child was otherwise ready and motivated. Usually in an older child or adolescent and always coupled with counseling.
3 Posts in Enuresis-Bed Wetting (enuresis) Series
- Urinary Tract Infections – 9 Apr 2015
- Part 2 - Bed wetting – 6 Jul 2013
- Part 1 - Bed wetting – 9 Jun 2013
Advertisement by Google
(sorry, only few pages have ads)